Page 1082 - TNFlipTest
P. 1082
P48 Pediatrics
Rochester Criteria – Developed to Identify Infants ≤60 d of Age with Fever at Low Risk of Serious Bacterial Infection
Infectious Diseases Toronto Notes 2019 • admittohospitalifappropriate
Management
• • • •
treatthesourceifknown replacefluidlosses(e.g.fromvomiting,diarrhea,etc.);maintenancefluidneedsarehigherinfebrilechild reassureparentsthatmostfeversarebenignandself-limited antipyretics(acetaminophenand/oribuprofen)arenotnecessaryinmostcases,butcanbegivenifchild is uncomfortable
Clinically WBC Count Bands Urinalysis Stool
(if diarrhea) Past Health
Well
5-15 x 109/L <1.5 x 109/L <10 WBC/HPF <5 WBC/HPF
Born >37 wk
Home with/before mom No hospitalizations
No prior antibiotic use No prior treatment
for unexplained hyperbilirubinemia
No chronic disease
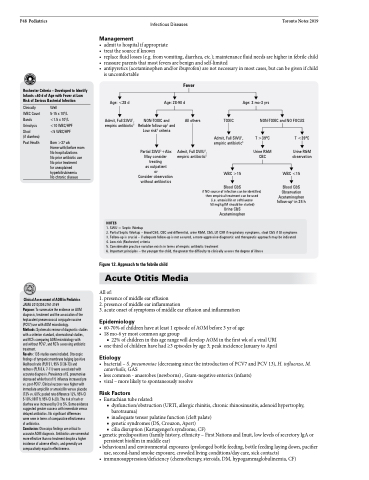
Age: <28 d
Admit, Full SWU1, empiric antibiotic5
Fever
Age: 28-90 d
Age: 3 mo-3 yrs
NON-TOXIC and NO FOCUS
NON-TOXIC and Reliable follow-up3 and Low risk4 criteria
Partial SWU2+Abx May consider treating
as outpatient
or Consider observation without antibiotics
All others
Admit, Full SWU1, empiric antibiotic5
TOXIC
Admit, Full SWU1, empiric antibiotic5
WBC >15
T >39oC
Urine R&M CBC
T <39oC
Urine R&M observation
WBC <15
Blood C&S Observation Acetaminophen follow-up3 in 24 h
Clinical Assessment of AOM in Pediatrics
JAMA 2010;304:2161-2169
Purpose: To summarize the evidence on AOM diagnosis, treatment and the association of the heptavalent pneumococcal conjugate vaccine (PCV7) use with AOM microbiology.
Methods: Systematic review of diagnostic studies with a criterion standard, observational studies, and RCTs comparing AOM microbiology with
and without PCV7, and RCTs assessing antibiotic treatment.
Results: 135 studies ewre included. Otoscopic findings of tympanic membrane bulging (positive likelihood ratio (PLR 51, 95% CI 36-73) and
redness (PLR 8.4, 7-11) were associated with accurate diagnosis. Prevalence of S. pneumoniae decreased while that of H. influenza increased pre vs. post-PCV7. Clinical success was higher with immediate ampicillin or amoxicillin versus placebo (73% vs. 60%; pooled rate difference 12%, 95% CI 5-18%; NNT 9, 95% CI 6-20). The risk of rash or diarrhea was increased by 3 to 5%. Some evidence suggested greater success with immediate versus delayed antibiotics. No significant differences
were seen in terms of comparative effectiveness
of antibiotics.
Conclusion: Otoscoipc findings are critical to accurate AOM diagnosis. Antibiotics are somewhat more effective than no treatment despite a higher incidence of adverse effects, and generally are comparatively equal in effectiveness.
Figure 12. Approach to the febrile child
Acute Otitis Media
All of:
1. presence of middle ear effusion
2. presence of middle ear inflammation
3. acute onset of symptoms of middle ear effusion and inflammation
Epidemiology
• 60-70%ofchildrenhaveatleast1episodeofAOMbefore3yrofage • 18mo-6yrmostcommonagegroup
■ 22% of children in this age range will develop AOM in the first wk of a viral URI • onethirdofchildrenhavehad≥3episodesbyage3;peakincidenceJanuarytoApril
Etiology
• bacterial–S.pneumoniae(decreasingsincetheintroductionofPCV7andPCV13),H.influenza,M. catarrhalis, GAS
• less common - anaerobes (newborns) , Gram-negative enterics (infants)
• viral–morelikelytospontaneouslyresolve
Risk Factors
• Eustachiantuberelated:
■ dysfunction/obstruction (URTI, allergic rhinitis, chronic rhinosinusitis, adenoid hypertrophy,
barotrauma)
■ inadequate tensor palatine function (cleft palate) ■ genetic syndromes (DS, Crouzon, Apert)
■ cilia disruption (Kartagenger’s syndrome, CF)
• genetic predisposition (family history, ethnicity – First Nations and Inuit, low levels of secretory IgA or persistent biofilm in middle ear)
• behavioural and environmental exposures (prolonged bottle feeding, bottle feeding laying down, pacifier use, second-hand smoke exposure, crowded living conditions/day care, sick contacts)
• immunosuppression/deficiency(chemotherapy,steroids,DM,hypogammaglobulinemia,CF)
NOTES
1. SWU = Septic Workup
2. Partial Septic Workup – blood C&S, CBC and differential, urine R&M, C&S, LP, CXR if respiratory symptoms, stool C&S if GI symptoms 3. Follow-up is crucial – if adequate follow-up is not assured, a more aggressive diagnostic and therapeutic approach may be indicated 4. Low-risk (Rochester) criteria
5. Considerable practice variation exists in terms of empiric antibiotic treatment
6. Important principles – the younger the child, the greater the difficulty to clinically assess the degree of illness
Blood C&S
if NO source of infection can be identified, then empirical treatment can be used (i.e. amoxicillin or ceftriaxone
50 mg/kg IM should be started) Urine C&S Acetaminophen