Page 1113 - TNFlipTest
P. 1113
Toronto Notes 2019 Respirology
• medication
■ initiate: treatment with drug appropriate to seizure type; often if >2 unprovoked afebrile seizures
within 6-12 mo
■ optimize: start with one drug and increase dosage until seizures controlled
■ if no effect, switch over to another before adding a second antiepileptic drug
■ continue antiepileptic drug therapy until patient free of seizures for >2 yr, then wean over 4-6 mo
• ketogenicdiet(highfatdiet):usedinpatientswhodonotrespondtopolytherapyorwhodonotwishto take medication (valproic acid contraindicated in conjunction with ketogenic diet because may increase hepatotoxicity)
• legalobligationtoreporttoMinistryofTransportationifpatientwishestodrive
Generalized and Partial Seizures
• seeNeurology,N18 Respirology
Asthma
Definition
• seeRespirology,R7
• inflammatorydisorderoftheairwaryscharacterizedbyrecurrentepisodesofreversiblesmallairway
obstruction, resulting from airway hyperresponsiveness to endogenous and exogenous stimuli
• verycommon,presentsmostofteninearlychildhood
• associated with other atopic diseases such as allergic rhinitis or atopic dermatitis
Clinical Presentation
• episodicboutsofwheezing,dyspnea,tachypnea,cough(usuallyatnight/earlymorning,withactivity,or cold exposure)
• physical exam may reveal hyper-resonant chest, prolonged expiration, wheeze
• symptoms may be exacerbated by “triggers”: URTI (viral or Mycoplasma), weather (cold exposure,
humidity changes), allergens (pets), irritants (cigarette smoke), exercise, emotional stress, drugs (ASA, β-blockers)
Classification
• mild:occasionalattacksofwheezingorcoughing(<2/wk);symptomsrespondquicklytoinhaled bronchodilator; never needs systemic corticosteroids
• moderate:morefrequentepisodeswithsymptomspersistingandchroniccough;decreasedexercise tolerance; sometimes needs systemic corticosteroids
• severe: daily and nocturnal symptoms; frequent ED visits and hospitalizations; usually needs systemic corticosteroids
Management
• acute
■ O2 (keep O2 saturation >94%) and fluids if dehydrated
■ β2-agonists: salbutamol (Ventolin®) MDI + spacer (nebulized or IV in very severe episodes with
impending respiratory failure), 5 puffs (<20 kg) or 10 puffs q20min for first h (>20 kg)
■ ipratropium bromide (Atrovent®) if severe: MDI + spacer, 3 puffs (<20 kg) or 6 puffs (>20 kg)
q20min with salbutamol, or add to first 3 salbutamol masks (0.25 mg if <20 kg, 0.5mg if >20 kg)
■ steroids: prednisone (1-2 mg/kg x 5 d) or dexamethasone (0.3 mg/kg/d x 5 d or 0.6 mg/kg/d x 2 d);
in severe disease, use IV steroids
■ if no response, add magnesium sulphate
■ continue to observe; can discharge patient if asymptomatic for 2-4 h after last dose
• chronic
■ education, emotional support, avoid allergens or irritants, develop an “action plan”
■ exercise program (e.g. swimming)
■ monitor respiratory function with peak flow meter (improves self-awareness of status)
■ PFTs for children >6 yr
■ reliever therapy: short acting β2-agonists (e.g. salbutamol)
■ controller therapy (first line therapy for all children): low dose daily inhaled corticosteroids
■ second line therapy for children <12 yr: moderate dose of daily inhaled corticosteoroids
■ second line therapy for children >12 yr: leukotriene receptor antagonist OR long acting β2-agonist
in conjunction with low dose inhaled corticosteroids; leukotriene receptor antagonist monotherapy
may be considered an alternative second line therapy
■ severe asthma unresponsive to first and second line treatments: injection immunotherapy ■ aerochamber for children using daily inhaled corticosteroids
• indicationsforhospitalization
■ ongoing need for supplemental O2
■ persistently increased work of breathing
■ β2-agonists are needed more often than q4h after 4-8 h of conventional treatment ■ patient deteriorates while on systemic steroids
Pediatrics P79
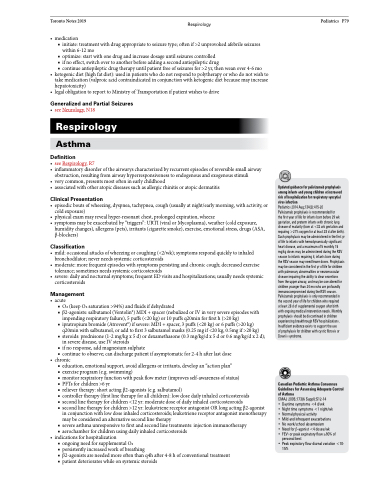
Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection
Pediatrics 2014 Aug;134(2):415-20
Palivizumab prophylaxis is recommended for
the first year of life for infants born before 29 wk gestation, and preterm infants with chronic lung disease of maturity (born at <32 wk gestation and requiring >21% oxygen for at least 28 d after birth). Such prophylaxis may be administered in the first yr of life to infants with hemodynamically significant heart disease, and a maximum of 5 monthly 15 mg/kg doses may be administered during the RSV season to infants requiring it; infants born during the RSV season may need fewer doses. Prophylaxis may be considered in the first yr of life for children with pulmonary abnormalities or neuromuscular disease impairing the ability to clear secretions from the upper airway, and may be considered for children younger than 24 mo who are profoundly immunocompromised during the RSV season. Palivizumab prophylaxis is only recommended in the second year of life for children who required
at least 28 d of supplemental oxygen after birth with ongoing medical intervention needs. Monthly prophylaxis should be discontinued in children experiencing breakthrough RSV hospitalizations. Insufficient evidence exists to support the use
of prophylaxis for children with cystic fibrosis or Down’s syndrome.
Canadian Pediatric Asthma Consensus Guidelines for Assessing Adequate Control of Asthma
CMAJ 2005;173(6 Suppl):S12-14
• Daytime symptoms <4 d/wk
• Night time symptoms <1 night/wk
• Normal physical activity
• Mild and infrequent exacerbations
• No work/school absenteeism
• Need for β-agonist <4 doses/wk
• FEV1 or peak expiratory flow ≥90% of
personal best
• Peak expiratory flow diurnal variation <10-
15%