Page 1121 - TNFlipTest
P. 1121
Toronto Notes 2019
Common Medications
Pediatrics P87
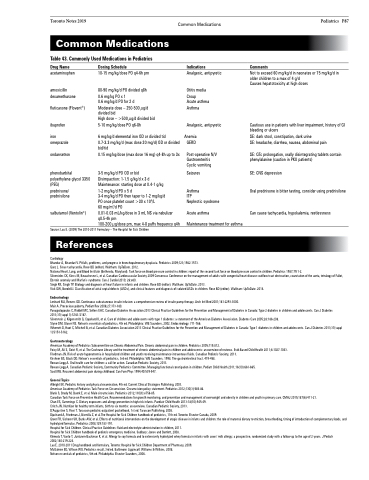
Common Medications
Table 43. Commonly Used Medications in Pediatrics
Drug Name
acetaminophen
amoxicillin dexamethasone
fluticasone (Flovent®)
ibuprofen
iron omeprazole
ondansetron
phenobarbital polyethylene glycol 3350 (PEG)
prednisone/
prednisilone
salbutamol (Ventolin®)
Dosing Schedule
10-15 mg/kg/dose PO q4-6h prn
80-90 mg/kg/d PO divided q8h 0.6 mg/kg PO x 1
0.6 mg/kg/d PO for 2 d Moderate dose – 250-500 μg/d divided bid
High dose – >500 μg/d divided bid 5-10 mg/kg/dose PO q6-8h
6 mg/kg/d elemental iron OD or divided tid
0.7-3.3 mg/kg/d (max dose 20 mg/d) OD or divided bid/tid
0.15 mg/kg/dose (max dose 16 mg) q4-8h up to 3x
3-5 mg/kg/d PO OD or bid
Disimpaction: 1-1.5 g/kg/d x 3 d
Maintenance: starting dose at 0.4-1 g/kg
1-2 mg/kg/d PO x 5 d
3-4 mg/kg/d PO then taper to 1-2 mg/kg/d
PO once platelet count >30 x 109/L
60 mg/m2/d PO
0.01-0.03 mL/kg/dose in 3 mL NS via nebulizer q0.5-4h prn
100-200 μg/dose prn, max 4-8 puffs frequency q4h
Indications
Analgesic, antipyretic
Otitis media Croup
Acute asthma Asthma
Analgesic, antipyretic
Anemia GERD
Post-operative N/V Gastroenteritis Cyclic vomiting
Seizures
Asthma
ITP
Nephrotic syndrome
Acute asthma
Maintenance treatment for asthma
Comments
Not to exceed 60 mg/kg/d in neonates or 75 mg/kg/d in older children to a max of 4 g/d
Causes hepatotoxicity at high doses
Cautious use in patients with liver impairment, history of GI bleeding or ulcers
SE: dark stool, constipation, dark urine
SE: headache, diarrhea, nausea, abdominal pain
SE: QTc prolongation, orally disintegrating tablets contain phenylalanine (caution in PKU patients)
SE: CNS depression
Oral prednisone is bitter tasting, consider using prednisilone
Can cause tachycardia, hypokalemia, restlessness
Source: Lau E. (2009) The 2010-2011 Formulary – The Hospital for Sick Children
References
Cardiology
Bhandar A, Bhandari V. Pitfalls, problems, and progress in bronchopulmonary dysplasia. Pediatrics 2009;123;1562-1573.
Ganz L. Sinus tachycardia. Rose BD (editor). Waltham: UpToDate. 2012.
National Heart, Lung, and Blood Institute (Bethesda, Maryland). Task force on blood pressure control in children: report of the second task force on blood pressure control in children. Pediatrics 1987;79:1-2.
Silversides CK, Kiess M, Beauchesne L, et al. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: outflow tract obstruction, coarctation of the aorta, tetralogy of Fallot, Ebstein anomaly and Marfan’s syndrome. Can J Cardiol 2010; 26:e80.
Singh RK, Singh TP. Etiology and diagnosis of heart failure in infants and children. Rose BD (editor). Waltham: UpToDate. 2013.
Vick GW, Bezold LI. Classification of atrial septal defects (ASDs), and clinical features and diagnosis of isolated ASDs in children. Rose BD (editor). Waltham: UpToDate. 2014.
Endocrinology
Lenhard MJ, Reeves GD. Continuous subcutaneous insulin infusion: a comprehensive review of insulin pump therapy. Arch Int Med 2001;161:2293-3000.
Muir A. Precocious puberty. Pediatr Rev 2006;27:373-380.
Panagiotopoulos C, Riddell MC, Sellers EAC. Canadian Diabetes Association 2013 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada: Type 2 diabetes in children and adolescents. Can J Diabetes 2013;37(suppl 1):S163-S167.
Silverstein J, Kilgensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care 2005;28:186-208.
Styne DM, Glaser NS. Nelson’s essentials of pediatrics, 4th ed. Philadelphia: WB Saunders, 2002. Endocrinology. 711-766.
Wherrett D, Huot C, Mitchell B, et al. Canadian Diabetes Association 2013 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada: Type 1 diabetes in children and adolescents. Can J Diabetes 2013;37(suppl 1):S153-S162.
Gastroenterology
American Academy of Pediatrics Subcommittee on Chronic Abdominal Pain. Chronic abdominal pain in children. Pediatrics 2005;115:812.
Foisy M, Ali S, Geist R, et al. The Cochrane Library and the treatment of chronic abdominal pain in children and adolescents: an overview of reviews. Evid-Based Child Health 2011;6:1027-1043. Friedman JN. Risk of acute hyponatremia in hospitalized children and youth receiving maintenance intravenous fluids. Canadian Pediatric Society, 2013.
Kirshner BS, Black DD. Nelson’s essentials of pediatrics, 3rd ed. Philadelphia: WB Saunders, 1998. The gastrointestinal tract. 419-458.
Rowan-Legg A. Oral health care for children: a call for action. Canadian Pediatric Society, 2013.
Rowan-Legg A. Canadian Pediatric Society, Community Pediatrics Committee. Managing functional constipation in children. Pediatr Child Health 2011;16(10):661-665.
Scott RB. Recurent abdominal pain during childhood. Can Fam Phys 1994;40:539-547.
General Topics
Albright EK. Pediatric history and physical examination, 4th ed. Current Clinical Strategies Publishing, 2003.
American Academy of Pediatrics Task Force on Circumcision. Circumcision policy statement. Pediatrics 2012;130(3):585-86.
Blank S, Brady M, Buerk E, et al. Male circumcision. Pediatrics 2012;130(3):e756-85.
Canadian Task Force on Preventive Health Care. Recommendations for growth monitoring, and prevention and management of overweight and obesity in children and youth in primary care. CMAJ 2015;187(6):411-21.
Chan ES, Cummings C. Dietary exposures and allergy prevention in high-risk infants. Paediatr Child Health 2013:18(10):545-49.
Critch JN. Nutrition for healthy term infants, birth to six months: an overview. Canadian Pediatric Society, 2013.
D’Augustine S, Flosi T. Tarascon pediatric outpatient pocketbook, 1st ed. Tarascon Publishing, 2008.
Dipchand A, Friedman J, Bismilla Z, et al.The Hospital for Sick Children handbook of pediatrics, 11th ed. Toronto: Elsevier Canada, 2009.
Greer FR, Sicherer SH, Burks AW, et al. Effects of nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics 2008;129:183-191.
Hospital for Sick Children. Clinical Practice Guidelines: fluid and electrolyte administration in children, 2011.
Hospital for Sick Children handbook of pediatric emergency medicine. Sudbury: Jones and Bartlett, 2008.
Klemola T, Vanto T, Juntunen-Backman K, et al. Allergy to soy formula and to extensively hydrolyzed whey formula in infants with cows’ milk allergy: a prospective, randomized study with a follow-up to the age of 2 years. J Pediatr 2002;140:219-224.
Lau E. 2010-2011 Drug handbook and formulary. Toronto: Hospital for Sick Children Department of Pharmacy, 2009.
McGahren ED, Wilson WG. Pediatrics recall, 3rd ed. Baltimore: Lippincott Williams & Wilkins, 2008.
Nelson essentials of pediatrics, 5th ed. Philadelphia: Elsevier Saunders, 2006.