Page 1192 - TNFlipTest
P. 1192
PS28 Psychiatry
Somatic Symptom and Related Disorders Toronto Notes 2019 Somatic Symptom Disorder
DSM-5 Diagnostic Criteria for Somatic Symptom Disorder
Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, 5th ed. 2013. American Psychiatric Association
A. one or more somatic symptoms that are distressing or result in significant disruption of daily life
B.
C. • •
• • • •
•
•
• • •
•
• • • •
excessive thoughts, feelings, or behaviours related to the somatic symptoms or associated health concerns as manifested by at least one of the following:
1. disproportionate and persistent thoughts about the seriousness of one’s symptoms 2. persistently high level of anxiety about health or symptoms
3. excessive time and energy devoted to these symptoms or health concerns
although any one somatic symptom may not be continuously present, the state of being symptomatic is persistent (typically >6 mo)
somatic symptom disorder with predominant pain (previously pain disorder) for those whose somatic symptom is primarily pain
patients have physical symptoms and believe these symptoms represent the manifestation of a serious illness
persistent belief despite negative medical investigations and may develop different symptoms over time lifetime prevalence may be around 5-7% in the general adult population
females tend to report more somatic symptoms than males do, cultural factors may influence sex ratio complications: anxiety and depression commonly comorbid (up to 80%), unnecessary medications or surgery
often a misdiagnosis for an insidious illness so rule out all organic illnesses (e.g. multiple sclerosis)
Illness Anxiety Disorder
preoccupation with fear of having, or the idea that one has, a serious disease, to the point of causing significant impairment
convictions persist despite negative investigations and medical reassurance
somatic symptoms are mild or not present
there is a high level of anxiety about health and the individual is easily alarmed about personal health status
person engages in maladaptive behaviour such as excessive physical checking or total healthcare avoidance
duration is ≥6 mo; onset in 3rd-4th decade of life
a new diagnostic entity so epidemiology is not well known; however, it is likely less common than SSD possible role for SSRIs due to generally high level of anxiety
specifiers: care-seeking type or care-avoidant type
Conversion Disorder (Functional Neurological Symptom Disorder)
la belle indifférence
An inappropriately cavalier patient attitude in the face of serious symptoms; classically associated with conversion disorder
• ≥1symptomsordeficitsaffectingvoluntarymotororsensoryfunctionthatmimicaneurologicalor GMC (e.g. impaired coordination, local paralysis, double vision, seizures, or convulsions)
• doesnotneedtobeprecededbyapsychologicaleventasperpreviousDSMcriteria,howeverthisisstill worth exploring as many patients will present after such an event or related to a medical diagnosis in a first-degree relative
• 2-5/100,000ingeneralpopulation;5%ofreferralstoneurologyclinics
• morecommoninruralpopulationsandinindividualswithlittlemedicalknowledge
• spontaneousremissionin95%ofacutecases,50%ofchroniccases(>6mo)
• incompatiblefindingsdetectedfromspecificneurologicaltestingcanhelpdifferentiatebetween
functional and neurological origin (e.g. Hoover’s sign and dermatome testing)
• specifiers:acuteepisode(<6mosymptomduration),chronicepisode(>6mosymptomduration),with
psychological stressor, without psychological stressor
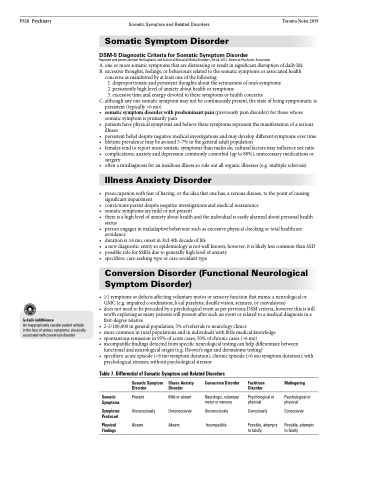
Table 7. Differential of Somatic Symptom and Related Disorders
Somatic Symptom Disorder
Present Unconsciously Absent
Conversion Disorder
Factitious Disorder
Psychological or physical
Consciously
Possible, attempts to falsify
Malingering
Psychological or physical
Consciously
Possible, attempts to falsify
Illness Anxiety Disorder
Mild or absent
Unconsciously Unconsciously Absent Incompatible
Somatic Symptoms
Symptoms Produced
Physical Findings
Neurologic, voluntary motor or sensory