Page 1202 - TNFlipTest
P. 1202
PS38 Psychiatry
Neurodevelopmental Disorders Toronto Notes 2019
• notbetterexplainedbyintellectualdisabilityorglobaldevelopmentaldelay • specifiers
■ current severity: requiring very substantial support, requiring substantial support, requiring support ■ ± language impairment, ± intellectual impairment
■ associated with known medical or genetic condition or environmental factor
Differential Diagnosis
• neurodevelopmental:globaldelay,intellectualdisability,languagedisorder,socialcommunication disorder, learning disorder, developmental coordination disorder
• mentalandbehavioural:ADHD,mooddisorder,anxietydisorder,selectivemutism,attachment disorder, ODD, conduct disorder, OCD, childhood schizophrenia
• conditionswithdevelopmentalregression:Rettsyndrome,epilepticencephalopathy(Landau-Kleffner) • other: hearing/visual impairment, abuse
Treatment
• team-based:school,psychologist,occupationaltherapist,physiotherapist,speechandlanguagetherapy, pediatrics, psychiatry
• psychosocial:familyeducationandsupport,schoolprogramming,behaviourmanagement,socialskills training
• treat concomitant disorders such as ADHD, tics, OCD, anxiety, depression, and seizure disorder • adjunctive pharmacotherapy (does not treat ASD itself): atypical antipsychotics (for irritability,
aggression, agitation, self-mutilation, tics), SSRIs (for anxiety, depression), stimulants (for associated inattention and hyperactivity)
Prognosis
• variable,butimproveswithearlyintervention • betterifIQ>60andabletocommunicate
Attention Deficit Hyperactivity Disorder
• prevalence:5-12%ofschool-agedchildren;M:F=4:1,althoughgirlsmaybeunder-diagnosed
• girlstendtohaveinattentive/distractiblesymptoms;boyshaveimpulsive/hyperactivesymptoms
Etiology
• genetic:75%heritability,dopaminecandidategenesDAT1,DRD4
• neurobiology:decreasedcatecholaminetransmission,lowprefrontalcortex(PFC)activity,increased
beta activity on EEG
• cognitive:developmentaldisability,poorinhibitorycontrol,andothererrorsofexecutivefunction
Diagnosis
• differential:learningdisorders,hearing/visualdefects,thyroid,atopicconditions,congenitalproblems (fetal alcohol syndrome, Fragile X), lead poisoning, history of head injury, traumatic life events (abuse)
• diagnosisrequires:onsetbeforeage12,persistentsymptoms≥6mo,symptomspresentinatleast two settings (i.e. home, school, work), interferes with academic, family, and social functioning, and is divided into 3 subtypes
■ combined type: ≥6 symptoms of inattention and ≥6 symptoms of hyperactivity-impulsivity ■ predominantly inattentive type: ≥6 symptoms of inattention
■ predominantly hyperactive-impulsive type: ≥6 symptoms of hyperactivity-impulsivity
■ for adolescents/adults age 17 and older, ≥5 symptoms required
• doesnotoccurexclusivelyduringthecourseofanotherpsychiatricdisorder
Efficacy and Safety of Selective Serotonin Reuptake Inhibitors, Serotonin-Norepinephrine Reuptake Inhibitors, and Placebo for Common Psychiatric Disorders Among Children and Adolescents: A Systematic Review and Meta-Analysis
JAMA Psychiatry. 2017 Oct 1;74(10):1011-1020
Purpose: Examine the relative efficacy and safety of SSRIs, SNRIs, and placebo for the treatment of depressive disorders (DDs), anxiety disorders (ADs), obsessive- compulsive disorder (OCD), and posttraumatic stress disorder (PTSD) in children and adolescents.
Methods: Meta-analysis of RCTs regarding use of SSRIs or SNRIs in youths with DD, AD, OCD, or PTSD. Effect sizes, calculated as standardized mean differences (Hedges g) and risk ratios (RRs) for adverse events, were assessed in a random-effects model.
Results: Thirty-six trials were eligible and analysis showed that SSRIs and SNRIs were more beneficial compared
with placebo (g=0.32; 95% CI, 0.25-0.40; P<.001). ADs (g=0.56; 95% CI, 0.40-0.72; P<.001) had larger between- group effect sizes than DDs (g=0.20; 95% CI, 0.13-0.27; P<.001). Patients with DDs exhibited significantly larger placebo responses (g=1.57; 95% CI, 1.36-1.78; P<.001) compared with those with ADs (g=1.03; 95% CI, 0.84- 1.21; P<.001). The SSRIs produced a relatively large effect size for ADs (g=0.71; 95% CI, 0.45-0.97; P<.001). Patients receiving an antidepressant versus a placebo reported significantly more treatment-emergent adverse events (RR, 1.07; 95% CI, 1.01-1.12; P=.01 or RR, 1.49; 95% CI, 1.22-1.82; P<.001, depending on the reporting method), severe adverse events (RR, 1.76; 95% CI, 1.34- 2.32; P<.001), and study discontinuation due to adverse events (RR, 1.79; 95% CI, 1.38-2.32; P<.001). Conclusion: Compared with placebo, SSRIs and SNRIs are more beneficial than placebo in children and adolescents; however, the benefit is small and disorder specific, yielding a larger drug-placebo difference for AD than for other conditions. Response to placebo is large, especially in DD. Severe adverse events are significantly more common with SSRIs and SNRIs than placebo.
Observe child for “ATENTION” features Annoying
Temperamental
Energetic
Noisy
Task incompletion Inattentive Oppositional Negativism
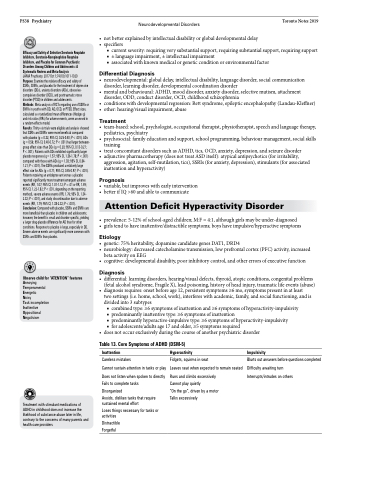
Table 13. Core Symptoms of ADHD (DSM-5)
Inattention
Careless mistakes
Cannot sustain attention in tasks or play
Does not listen when spoken to directly
Fails to complete tasks
Disorganized
Avoids, dislikes tasks that require sustained mental effort
Loses things necessary for tasks or activities
Distractible Forgetful
Hyperactivity
Fidgets, squirms in seat
Leaves seat when expected to remain seated
Runs and climbs excessively Cannot play quietly
“On the go”, driven by a motor Talks excessively
Impulsivity
Blurts out answers before questions completed Difficulty awaiting turn
Interrupts/intrudes on others
Treatment with stimulant medications of ADHD in childhood does not increase the likelihood of substance abuse later in life, contrary to the concerns of many parents and health care providers