Page 1297 - TNFlipTest
P. 1297
Toronto Notes 2019 Connective Tissue Disorders
Systemic Lupus Erythematosus
• seeNephrology,NP23
Definition
• chronicinflammatorymulti-systemdiseaseofunknownetiology
• characterizedbyproductionofautoantibodiesanddiverseclinicalmanifestations
Table 14. Diagnostic Criteria of SLE*
Rheumatology RH11
Criteria
CLINICAL
Malar rash
Discoid rash Photosensitivity Oral/nasal ulcers Arthritis
Serositis Neurologic disorder LABORATORY Renal disorder
Hematologic disorder Immunologic disorder
ANA
Description
Classic “butterfly rash”, sparing of nasolabial folds, no scarring May cause scarring due to invasion of basement membrane Skin rash in reaction to sunlight
Usually painless
Symmetric, involving ≥2 small or large peripheral joints, non-erosive Pleuritis or pericarditis
Headache, seizures or psychosis, peripheral neuropathies
Proteinuria (>0.5 g/d or 3+)
Cellular casts (RBC, Hb, granular, tubular, mixed)
Hemolytic anemia, leukopenia, lymphopenia, thrombocytopenia
Anti-dsDNA or anti-Sm or antiphospholipid Ab (anticardiolipin Ab, SLE anticoagulant) or false positive VDRL with 6 mo confirmatory negative
Most sensitive test (98%), not specific
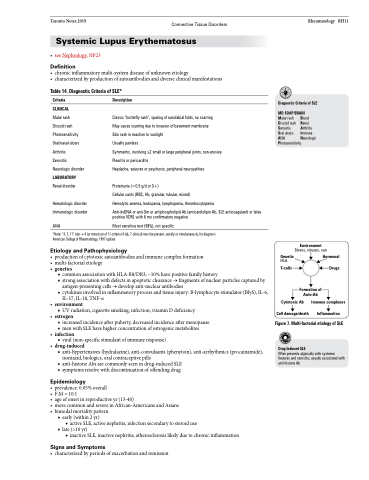
Diagnostic Criteria of SLE MD SOAP BRAIN
Malar rash Discoid rash Serositis
Oral ulcers ANA Photosensitivity
Blood Renal Arthritis Immune Neurologic
*Note: “4, 7, 11” rule → 4 (or more) out of 11 criteria (4 lab, 7 clinical) must be present, serially or simultaneously, for diagnosis American College of Rheumatology, 1997 update
Etiology and Pathophysiology
• productionofcytotoxicautoantibodiesandimmunecomplexformation Genetic
HLA
Environment
Stress, viruses, sun
• multi-factorialetiology
• genetics T-cells
■ common association with HLA-B8/DR3; ~10% have positive family history
■ strong association with defects in apoptotic clearance → fragments of nuclear particles captured by
antigen-presenting cells → develop anti-nuclear antibodies
■ cytokines involved in inflammatory process and tissue injury: B-lymphocyte stimulator (BlyS), IL-6,
IL-17, IL-18, TNF-α • environment
■ UV radiation, cigarette smoking, infection, vitamin D deficiency • estrogen
■ increased incidence after puberty, decreased incidence after menopause
■ men with SLE have higher concentration of estrogenic metabolites • infection
■ viral (non-specific stimulant of immune response) • drug-induced
■ anti-hypertensives (hydralazine), anti-convulsants (phenytoin), anti-arrhythmics (procainamide), isoniazid, biologics, oral contraceptive pills
■ anti-histone Abs are commonly seen in drug-induced SLE
■ symptoms resolve with discontinuation of offending drug
Epidemiology
• prevalence:0.05%overall
• F:M=10:1
• ageofonsetinreproductiveyr(13-40)
• morecommonandsevereinAfrican-AmericansandAsians • bimodalmortalitypattern
■ early (within 2 yr)
◆ active SLE, active nephritis, infection secondary to steroid use
■ late (>10 yr)
◆ inactive SLE, inactive nephritis, atherosclerosis likely due to chronic inflammation
Signs and Symptoms
• characterizedbyperiodsofexacerbationandremission
Hormonal
Drugs
Formation of Auto-Ab
Cytotoxic Ab
Cell damage/death
Figure 7. Multi-factorial etiology of SLE
Drug-Induced SLE
Often presents atypically with systemic features and serositis; usually associated with anti-histone Ab
Immune complexes
Inflammation