Page 1303 - TNFlipTest
P. 1303
Toronto Notes 2019 Vasculitides Overlap Syndrome
• syndromewithsufficientdiagnosticfeaturesof2+differentconnectivetissuediseases
Vasculitides
• inflammationandsubsequentnecrosisofbloodvesselsleadingtotissueischemiaorinfarctionofany organ system
• diagnosis
■ clinical suspicion: suspect in cases of unexplained multiple organ ischemia or systemic illness
with no evidence of malignancy or infection; constitutional symptoms such as fever, weight loss,
anorexia, fatigue
■ labs non-specific: anemia, increased WBC and ESR, abnormal U/A
■ investigations: biopsy if tissue accessible; angiography if tissue inaccessible
• treatmentgenerallyinvolvescorticosteroidsand/orimmunosuppressiveagents
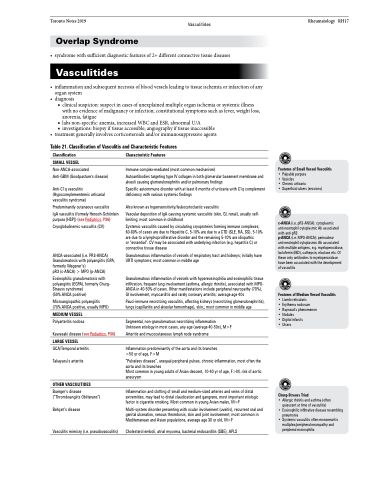
Table 21. Classification of Vasculitis and Characteristic Features
Rheumatology RH17
Classification
SMALL VESSEL Non-ANCA-associated
Anti-GBM (Goodpasture's disease)
Anti-C1q vasculitis (Hypocomplementemic urticarial vasculitis syndrome)
Predominantly cutaneous vasculitis
IgA vasculitis (formely Henoch-Schönlein purpura [HSP]) (see Pediatrics, P86)
Cryoglobulinemic vasculitis (CV)
ANCA-associated (i.e. PR3-ANCA) Granulomatosis with polyangiitis (GPA, formerly Wegener’s)
pR3 (c-ANCA) > MPO (p-ANCA)
Eosinophilic granulomatosis with polyangiitis (EGPA), formerly Churg- Strauss syndrome)
(50% ANCA positive)
Microangiopathic polyangiitis (70% ANCA positive, usually MPO)
MEDIUM VESSEL
Polyarteritis nodosa
Kawasaki disease (see Pediatrics, P86) LARGE VESSEL
GCA/Temporal arteritis
Takayasu’s arteritis
OTHER VASCULITIDES
Buerger’s disease (“Thromboangiits Obliterans”)
Behçet’s disease
Vasculitis mimicry (i.e. pseudovasculitis)
Characteristic Features
Immune complex-mediated (most common mechanism)
Autoantibodies targeting type IV collagen in both glomerular basement membrane and alveoli causing glomerulonephritis and/or pulmonary findings
Specific autoimmune disorder with at least 6 months of urticaria with C1q complement deficiency with various systemic findings
Also known as hypersensitivity/leukocytoclastic vasculitis
Vascular deposition of IgA causing systemic vasculitis (skin, GI, renal), usually self- limiting; most common in childhood
Systemic vasculitis caused by circulating cryoproteins forming immune complexes; 60-80% of cases are due to Hepatitis C, 5-10% are due to a CTD (SLE, RA, SS), 5-10% are due to a lymphoproliferative disorder and the remaining 5-10% are idiopathic
or “essential”. CV may be associated with underlying infection (e.g. hepatitis C) or connective tissue disease
Granulomatous inflammation of vessels of respiratory tract and kidneys; initially have URTI symptoms; most common in middle age
Granulomatous inflammation of vessels with hypereosinophilia and eosinophilic tissue infiltration, frequent lung involvement (asthma, allergic rhinitis), associated with MPO- ANCA in 40-50% of cases. Other manifestations include peripheral neuropathy (70%), GI involvement, myocarditis and rarely coronary arteritis; average age 40s
Pauci-immune necrotizing vasculitis, affecting kidneys (necrotizing glomerulonephritis), lungs (capillaritis and alveolar hemorrhage), skin,; most common in middle age
Segmental, non-granulomatous necrotizing inflammation Unknown etiology in most cases, any age (average 40-50s), M>F
Arteritis and mucocutaneous lymph node syndrome
Inflammation predominantly of the aorta and its branches >50 yr of age, F>M
“Pulseless disease”, unequal peripheral pulses, chronic inflammation, most often the aorta and its branches
Most common in young adults of Asian descent, 10-40 yr of age, F>M, risk of aortic aneurysm
Inflammation and clotting of small and medium-sized arteries and veins of distal extremities, may lead to distal claudication and gangrene, most important etiologic factor is cigarette smoking. Most common in young Asian males, M>F
Multi-system disorder presenting with ocular involvement (uveitis), recurrent oral and genital ulceration, venous thrombosis, skin and joint involvement; most common in Mediterranean and Asian populations, average age 30 yr old, M>F
Cholesterol emboli, atrial myxoma, bacterial endocarditis (SBE), APLS
Features of Small Vessel Vasculitis
• Palpable purpura
• Vesicles
• Chronic urticaria
• Superficial ulcers (erosions)
c-ANCA (i.e. pR3-ANCA): cytoplasmic anti-neutrophil cytoplasmic Ab associated with anti-pR3
p-ANCA (i.e. MPO-ANCA): perinuclear anti-neutrophil cytoplasmic Ab associated with multiple antigens, e.g. myeloperoxidase, lactoferrin (IBD), cathepsin, elastase etc. Of these only antibodies to myeloperoxidase have been associated with the development of vasculitis
Features of Medium Vessel Vasculitis
• Livedo reticularis
• Erythema nodosum
• Raynaud’s phenomenon • Nodules
• Digital infarcts
• Ulcers
Churg-Strauss Triad
• Allergic rhinitis and asthma (often quiescent at time of vasculitis)
• Eosinophilic infiltrative disease resembling pneumonia
• Systemic vasculitis often mononeuritis multiplex/peripheral neuropathy and peripheral eosinophilia