Page 1330 - TNFlipTest
P. 1330
U12 Urology
Overactive Bladder
Toronto Notes 2019
Post-Obstructive Diuresis
Definition
• polyuriaresultingfromreliefofobstructiveuropathy(i.e.elevatedcreatinine) • >3L/24hor>200cc/hovereachoftwoconsecutivehours
Pathophysiology
• physiologicPODsecondarytoexcretionofretainedurea,Na+,andH2O(highosmoticload)afterrelief of obstruction
■ self-limiting; usually resolves in 48 h with PO fluids but may persist to pathologic POD
• pathologicPODisaNa+-wastingnephropathysecondarytoimpairedconcentratingabilityoftherenal
tubules due to:
■ decreased reabsorption of NaCl in the thick ascending limb and urea in the collecting tubule ■ increased medullary blood flow (solute washout)
■ increased flow and solute concentration in the distal nephrons
Management
• admit patient and closely monitor hemodynamic status and electrolytes (Na+ and K+ q6-12h and replace prn; follow Cr and BUN to baseline)
• monitorU/Oq2handensuretotalfluidintake<U/Obyreplacingevery1mLU/Owith0.5mL1/2NS IV (PO fluids if physiologic POD)
• avoidglucose-containingfluidreplacement(iatrogenicdiuresis)
Overactive Bladder
Definition
• asymptomcomplexthatincludesurinaryurgencywithorwithouturgencyincontinence,urinaryfrequency (voiding ≥8 times in a 24 hr period), and nocturia (awakening ONE or more times at night to void)
Etiology
• multipleetiologiesproposed(neurogenic,myogenic,idiopathic)
• symptomsusuallyassociatedwithinvoluntarycontractionsofthedetrusormuscle
• maybeassociatedwithotherconditionssuchasSUIinwomenandBPHinmen(seeTable5)
Epidemiology
• F:M=1:1
• prevalenceincreaseswithage.42%inmales≥75years;31%infemales≥75years • womenexperienceincontinencemorecommonlythanmen
Diagnosis
• thediagnosticprocessshoulddocumentsymptomsthatdefineoveractivebladderandexcludeother disorders that could cause of the patient’s symptoms
• minimalrequirementsfortheprocessconsistof:
■ focused history including past genitourinary disorders and conditions outlined in Table 8,
questionnaires of LUTS and diaries of urination frequency, volume and pattern ■ P/E including genitourinary, pelvic and rectal examination
■ U/A to rule out hematuria and infection
• insomepatients,thefollowinginvestigationscouldbeconsidered
■ post-void residual
■ cystoscopy to rule out recurrent infections, carcinoma in situ and other intravesical abnormalities
• urodynamicstoruleoutobstructioninoldermen
Treatment
• non-pharmacological:behaviourtherapiessuchasbladdertraining,bladdercontrolstrategies,pelvicfloor muscle training, fluid management, and avoidance of caffeine, alcohol
• pharmacological(seeTable29)
■ anti-muscarinics: oxybutynin hydrochloride, tolterodine, solifenacin, fesoterodine, or trospium ■ β3-adrenoceptor agonist: mirabegron
• refractorypatientsmaybetreatedwith:
■ neuromuscular-junction inhibition: botulinum toxin bladder injection
• others
■ percutaneoustibialnervestimulation(notusedcommonlyinCanada) ■ sacralneuromodulation
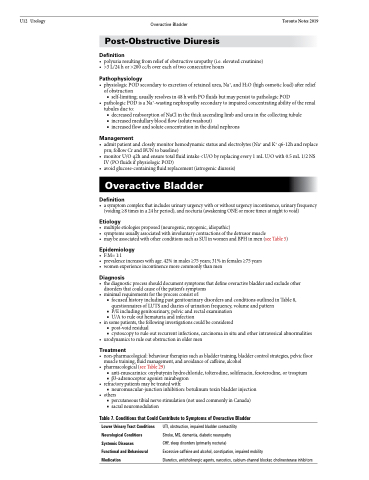
Table 7. Conditions that Could Contribute to Symptoms of Overactive Bladder
Lower Urinary Tract Conditions Neurological Conditions Systemic Diseases
Functional and Behavioural Medication
UTI, obstruction, impaired bladder contractility
Stroke, MS, dementia, diabetic neuropathy
CHF, sleep disorders (primarily nocturia)
Excessive caffeine and alcohol, constipation, impaired mobility
Diuretics, anticholinergic agents, narcotics, calcium-channel blocker, cholinesterase inhibitors