Page 211 - TNFlipTest
P. 211
Toronto Notes 2019 Medical Emergencies
Atrial Fibrillation
• mostcommonsustaineddysrhythmia;noorganizedPwaves(atrialrate>300/min),irregularlyirregular heart rate, narrow QRS (typically)
• etiology:HTN,CAD,thyrotoxicosis,EtOH(holidayheart),valvulardisease,pericarditis, cardiomyopathy, sick sinus syndrome
• treatment principles: stroke prevention, treat symptoms, identify/treat underlying cause
• decreasescardiacoutputby20-30%(duetolossoforganizedatrialcontractions)
• acutemanagement
■ if unstable: immediate synchronized cardioversion
■ if onset of AFib is >48 h: rate control, anticoagulate 3 wk prior to and 4 wk after cardioversion, or do
transesophageal echocardiogram to rule out clot
■ if onset <48 h or already anticoagulated: may cardiovert
◆ electrical cardioversion: synchronized direct current (DC) cardioversion
◆ chemical cardioversion: procainamide, flecainide, propafenone
• long-term management: rate or rhythm control, consider anticoagulation (CHADS2 score, see
Cardiology and Cardiac Surgery, C20)
Ventricular Tachydysrhythmias (wide QRS)
• VTach(rateusually140-200bpm)
■ definition: 3 or more consecutive ventricular beats at >100 bpm ■ etiology: CAD with MI is most common cause
■ treatment: sustained VTach (>30 s) is an emergency
◆ hemodynamic compromise: synchronized DC cardioversion
◆ no hemodynamic compromise: synchronized DC cardioversion, amiodarone, procainamide • VFib:callacodeblue,followACLSforpulselessarrest
• Torsadesdepointes
■ lookslikeVTachbutQRS‘rotatesaroundbaseline’withchangingaxisandamplitude(twistedribbon)
■ etiology: prolonged QT due to drugs (e.g. quinidine, TCAs, erythromycin, quinolones), electrolyte
imbalance (hypokalemia, hypomagnesemia), congenital
■ treatment
◆ IV Mg2+, temporary overdrive pacing, isoproterenol ◆ correct cause of prolonged QT
Acute Exacerbation of COPD (AECOPD)
• forchronicmanagementofCOPDseeRespirology,R9
• progressivedevelopmentofirreversibleairwayobstruction,typicallycausedbysmoking
History and Physical Exam
• cardinalsymptomsofAECOPD:increaseddyspnea,increasedcoughingfrequencyorseverity, increased sputum volume or purulence
• triggers:virus,pneumonia,urinarytractinfection,PE,CHF,MI,drugs
• characterizepreviousepisodesandhospitalizations,smokinghistory
• vital signs, LOC, signs of respiratory distress, respiratory exam
Investigations
• CBC,electrolytes,CXR,ECG,considerABG
• PFTsareNOTusefulinmanagingacuteexacerbations
Management
• oxygen:keepO2sat88-92%(beawarewhengivingO2tochronichypercapnic/CO2retainersbutdonot withhold O2 if hypoxic)
Emergency Medicine ER31
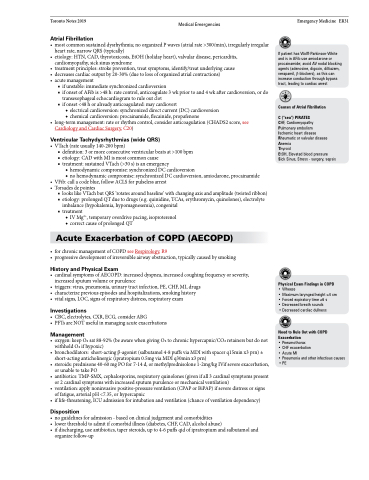
If patient has Wolff-Parkinson-White and is in AFib use amiodarone or procainamide; avoid AV nodal blocking agents (adenosine, digoxin, diltiazem, verapamil, β-blockers), as this can increase conduction through bypass tract, leading to cardiac arrest
Causes of Atrial Fibrillation
C (“sea”) PIRATES
CHF, Cardiomyopathy Pulmonary embolism Ischemic heart disease Rheumatic or valvular disease Anemia
Thyroid
EtOH, Elevated blood pressure Sick Sinus, Stress - surgery, sepsis
• bronchodilators: short-acting β-agonist (salbutamol 4-8 puffs via MDI with spacer q15min x3 prn) ± short-acting anticholinergic (ipratropium 0.5mg via MDI q30min x3 prn)
Physical Exam Findings in COPD
• Wheeze
• Maximum laryngeal height ≤4 cm • Forced expiratory time ≥6 s
• Decreased breath sounds
• Decreased cardiac dullness
Need to Rule Out with COPD Exacerbation
• Pneumothorax
• CHF exacerbation
• Acute MI
• Pneumonia and other infectious causes
•PE
• steroids:prednisone40-60mgPOfor7-14d,ormethylprednisolone1-2mg/kgIVifsevereexacerbation, or unable to take PO
• antibiotics:TMP-SMX,cephalosporins,respiratoryquinolones(givenifall3cardinalsymptomspresent or 2 cardinal symptoms with increased sputum purulence or mechanical ventilation)
• ventilation:applynoninvasivepositive-pressureventilation(CPAPorBiPAP)ifseveredistressorsigns of fatigue, arterial pH <7.35, or hypercapnic
• iflife-threatening,ICUadmissionforintubationandventilation(chanceofventilationdependency)
Disposition
• noguidelinesforadmission-basedonclinicaljudgementandcomorbidities
• lowerthresholdtoadmitifcomorbidillness(diabetes,CHF,CAD,alcoholabuse)
• ifdischarging,useantibiotics,tapersteroids,upto4-6puffsqidofipratropiumandsalbutamoland
organize follow-up