Page 22 - TNFlipTest
P. 22
ELOM8 Ethical, Legal, and Organizational Medicine Ethical and Legal Issues in Canadian Medicine Toronto Notes 2019
4 Basic Elements of Consent
• Voluntary • Capable • Specific • Informed
Four Basic Requirements of Valid Consent
1. Voluntary
■ consent must be given free of coercion or pressure (e.g. from parents or other family members who might exert ‘undue influence’)
■ the physician must not deliberately mislead the patient about the proposed treatment
2. Capable
■ the patient must be able to understand and appreciate the nature and effect of the proposed treatment
3. Specific
■ the consent provided is specific to the procedure being proposed and to the provider who will carry out the procedure (e.g. the patient must be informed if students will be involved in providing the treatment)
4. Informed
■ sufficient information and time must be provided to allow the patient to make choices in accordance with his/her wishes, including:
◆ the nature of the treatment or investigation proposed and its expected effects
◆ all significant risks and special or unusual risks
◆ alternative treatments or investigations and their anticipated effects and significant risks
◆ the consequences of declining treatment
◆ answers to any questions the patient may have
◆ the reasonable person test – the physician must provide all information that would be needed
“by a reasonable person in the patient’s position” to be able to make a decision
◆ disclose common adverse events and all serious risks (e.g. death), even if remote
◆ it is the physician’s responsibility to make reasonable attempts to ensure that the patient
understands the information, including overcoming language barriers, or communication
challenges
◆ physicians have a duty to inform the patient of all legitimate therapeutic options and must
not withhold information based on conscientious objections (e.g. not discussing the option of emergency contraception)
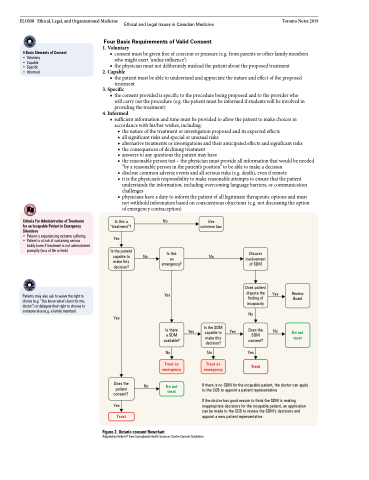
Criteria For Administration of Treatment for an Incapable Patient in Emergency Situations
• Patient is experiencing extreme suffering
• Patient is at risk of sustaining serious
bodily harm if treatment is not administered promptly (loss of life or limb)
Patients may also ask to waive the right to choice (e.g. “You know what’s best for me, doctor”) or delegate their right to choose to someone else (e.g. a family member)
Is this a “treatment”?
Yes
Is the patient capable to make this decision?
Yes
Does the patient consent?
Yes
Treat
No
No
Is this an emergency?
Yes
Is there a SDM available?
No
Treat as emergency
Do not treat
Use common law
No
Is the SDM capable to make this decision?
No
Treat as emergency
Discuss involvement of SDM
Does patient dispute the Yes
finding of incapacity
No
Does the No
SDM consent?
Yes
Treat
Yes
Yes
Review Board
Do not treat
No
If there is no SDM for the incapable patient, the doctor can apply to the CCB to appoint a patient representative
If the doctor has good reason to think the SDM is making inappropriate decisions for the incapable patient, an application can be made to the CCB to review the SDM’s decisions and appoint a new patient representative
Figure 2. Ontario consent flowchart
Adapted by Hébert P from Sunnybrook Health Sciences Centre Consent Guidelines