Page 275 - TNFlipTest
P. 275
Toronto Notes 2019 Adrenal Cortex Cushing’s Syndrome
Definition
• resultsfromchronicglucocorticoidexcess(endogenousorexogenoussources)
Etiology
• ACTH-dependent(85%)–bilateraladrenalhyperplasiaandhypersecretiondueto:
■ ACTH-secreting pituitary adenoma (Cushing’s disease; 80% of ACTH-dependent)
■ ectopic ACTH-secreting tumour (e.g. small cell lung carcinoma, bronchial, carcinoid, pancreatic
islet cell, pheochromocytoma, or medullary thyroid tumours) • ACTH-independent(15%)
■ long-term use of exogenous glucocorticoids
■ primary adrenocortical tumours: adenoma and carcinoma (uncommon) ■ bilateral adrenal nodular hyperplasia
Clinical Features
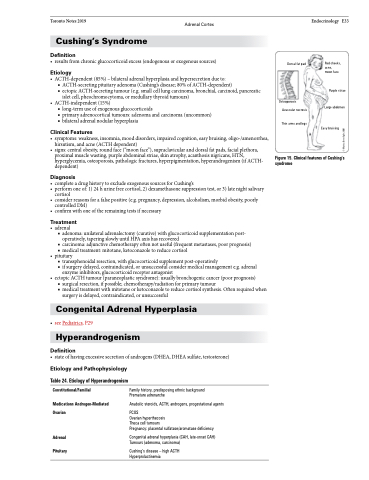
• symptoms:weakness,insomnia,mooddisorders,impairedcognition,easybruising,oligo-/amenorrhea, hirsutism, and acne (ACTH dependent)
• signs:centralobesity,roundface(“moonface”),supraclavicularanddorsalfatpads,facialplethora, proximal muscle wasting, purple abdominal striae, skin atrophy, acanthosis nigricans, HTN, hyperglycemia, osteoporosis, pathologic fractures, hyperpigmentation, hyperandrogenism (if ACTH- dependent)
Diagnosis
• completeadrughistorytoexcludeexogenoussourcesforCushing’s
• performoneof:1)24hurinefreecortisol,2)dexamethasonesuppressiontest,or3)latenightsalivary
cortisol
• considerreasonsforafalsepositive(e.g.pregnancy,depression,alcoholism,morbidobesity,poorly
controlled DM)
• confirmwithoneoftheremainingtestsifnecessary
Treatment
• adrenal
■ adenoma: unilateral adrenalectomy (curative) with glucocorticoid supplementation post-
operatively, tapering slowly until HPA axis has recovered
■ carcinoma: adjunctive chemotherapy often not useful (frequent metastases, poor prognosis) ■ medical treatment: mitotane, ketoconazole to reduce cortisol
• pituitary
■ transsphenoidal resection, with glucocorticoid supplement post-operatively
■ if surgery delayed, contraindicated, or unsuccessful consider medical management e.g. adrenal
enzyme inhibitors, glucocorticoid receptor antagonist
• ectopicACTHtumour(paraneoplasticsyndrome):usuallybronchogeniccancer(poorprognosis)
■ surgical resection, if possible; chemotherapy/radiation for primary tumour
■ medical treatment with mitotane or ketoconazole to reduce cortisol synthesis. Often required when
surgery is delayed, contraindicated, or unsuccessful
Congenital Adrenal Hyperplasia
• seePediatrics,P29 Hyperandrogenism
Definition
• stateofhavingexcessivesecretionofandrogens(DHEA,DHEAsulfate,testosterone)
Dorsal fat pad
Osteoporosis Avascular necrosis
Thin arms and legs
Endocrinology E33
Red cheeks, acne,
moon face
Purple striae Large abdomen
Easy bruising
Figure 15. Clinical features of Cushing’s syndrome
Etiology and Pathophysiology
Table 24. Etiology of Hyperandrogenism
Constitutional/Familial
Medications Androgen-Mediated Ovarian
Adrenal Pituitary
Family history, predisposing ethnic background Premature adrenarche
Anabolic steroids, ACTH, androgens, progestational agents
PCOS
Ovarian hyperthecosis
Theca cell tumours
Pregnancy: placental sulfatase/aromatase deficiency
Congenital adrenal hyperplasia (CAH, late-onset CAH) Tumours (adenoma, carcinoma)
Cushing’s disease – high ACTH Hyperprolactinemia
© Marisa Bonofiglio 2001