Page 327 - TNFlipTest
P. 327
Toronto Notes 2019
Common Presenting Problems
Family Medicine FM29
Epistaxis
• seeOtolaryngology,OT26
Erectile Dysfunction
• seeUrology,U32
Definition
• consistentorrecurrentinabilitytoattainand/ormaintainpenileerectionsufficientforsexual performance of ≥3 mo duration
Epidemiology
• ~20%ofmenage40;~50%ofmenage70
Etiology
• organic:vascular(90%)(arterialinsufficiency,atherosclerosis),endocrine(lowtestosterone,DM), anatomic (structural abnormality, e.g. Peyronie’s), neurologic (post-operative, DM), medications (clonidine, antihypertensives, psychotropics)
• psychogenic(10%)
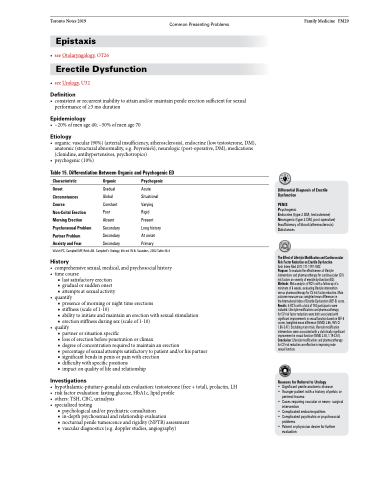
Table 15. Differentiation Between Organic and Psychogenic ED
Characteristic
Onset
Circumstances
Course
Non-Coital Erection Morning Erection Psychosexual Problem Partner Problem Anxiety and Fear
Organic
Gradual Global Constant Poor Absent Secondary Secondary Secondary
Psychogenic
Acute Situational Varying Rigid Present Long history At onset Primary
Differential Diagnosis of Erectile Dysfunction
PENIS
Psychogenic
Endocrine (type 2 DM, testosterone) Neurogenic (type 2 DM, post-operative) Insufficiency of blood (atherosclerosis) Substances
The Effect of Lifestyle Modification and Cardiovascular Risk Factor Reduction on Erectile Dysfunction
Arch Intern Med 2011;171:1797-1803
Purpose: To evaluate the effectiveness of lifestyle interventions and pharmacotherapy for cardiovascular (CV) risk factors on severity of erectile dysfunction (ED). Methods: Meta-analysis of RCTs with a follow-up of a minimum of 6 weeks, evaluating lifestyle intervention versus pharmacotherapy for CV risk factor reduction. Main outcome measure was weighted mean differences in
the International Index of Erectile Dysfunction (IIEF-5) score. Results: 6 RCTs with a total of 740 participants were included. Lifestyle modifications and pharmacotherapy
for CV risk factor reduction were both associated with significant improvements in sexual function based on IIEF-5 scores (weighted mean difference (WMD) 2.66, 95% CI 1.86-3.47). Excluding statin trials, lifestyle modification interventions were associated with a statistically significant improvement in sexual function (WMD 2.40, 1.19-3.61). Conclusion: Lifestyle modifications and pharmacotherapy for CV risk reduction are effective in improving male
sexual function.
Reasons for Referral to Urology
• Significant penile anatomic disease
• Younger patient with a history of pelvic or
perineal trauma
• Cases requiring vascular or neuro- surgical
intervention
• Complicated endocrinopathies
• Complicated psychiatric or psychosocial
problems
• Patient or physician desire for further
evaluation
Walsh PC, Campbell MF, Retik AB. Campbell’s Urology, 8th ed. W.B. Saunders, 2002.Table 46-4
History
• comprehensivesexual,medical,andpsychosocialhistory • timecourse
■ last satisfactory erection ■ gradual or sudden onset ■ attempts at sexual activity
• quantify
■ presence of morning or night time erections
■ stiffness (scale of 1-10)
■ ability to initiate and maintain an erection with sexual stimulation ■ erection stiffness during sex (scale of 1-10)
• qualify
■ partner or situation specific
■ loss of erection before penetration or climax
■ degree of concentration required to maintain an erection
■ percentage of sexual attempts satisfactory to patient and/or his partner ■ significant bends in penis or pain with erection
■ difficulty with specific positions
■ impact on quality of life and relationship
Investigations
• hypothalamic-pituitary-gonadalaxisevaluation:testosterone(free+total),prolactin,LH • riskfactorevaluation:fastingglucose,HbA1c,lipidprofile
• others: TSH, CBC, urinalysis
• specializedtesting
■ psychological and/or psychiatric consultation
■ in-depth psychosexual and relationship evaluation
■ nocturnal penile tumescence and rigidity (NPTR) assessment ■ vascular diagnostics (e.g. doppler studies, angiography)