Page 358 - TNFlipTest
P. 358
G8 Gastroenterology
Esophagus
Toronto Notes 2019
Remember:
Dysphagia = Difficulty in swallowing Odynophagia = Pain on swallowing
Key Questions in Dysphagia
• Difficulty in starting swallowing?
• Associated symptoms? (regurgitation,
change in voice pitch, weight loss)
• Solids, liquids, or both?
• Intermittent or progressive?
• History of heartburn?
• Change in eating habits/diet?
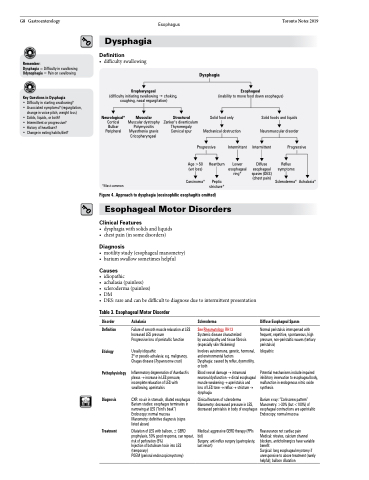
Dysphagia
Definition
• difficultyswallowing
Oropharyngeal
(difficulty initiating swallowingchoking, coughing, nasal regurgitation)
Dysphagia
Esophageal
(inability to move food down esophagus)
Neurological*
Cortical Bulbar Peripheral
*Most common
Muscular
Muscular dystrophy Polymyositis Myasthenia gravis Cricopharyngeal
Structural
Zenker’s diverticulum Thyromegaly Cervical spur
Solid food only
Mechanical obstruction
Solid foods and liquids
Neuromuscular disorder
Progressive
Intermittent Intermittent
Progressive
Reflux symptoms
Scleroderma* Achalasia*
Age >50 (wt loss)
Carcinoma*
Heartburn
Peptic stricture*
Lower esophageal ring*
Diffuse esophageal spasm (DES) (chest pain)
Figure 4. Approach to dysphagia (eosinophilic esophagitis omitted)
Esophageal Motor Disorders
Clinical Features
• dysphagiawithsolidsandliquids • chestpain(insomedisorders)
Diagnosis
• motilitystudy(esophagealmanometry) • bariumswallowsometimeshelpful
Causes
• idiopathic
• achalasia(painless)
• scleroderma(painless)
• DM
• DES:rareandcanbedifficulttodiagnoseduetointermittentpresentation
Table 3. Esophageal Motor Disorder
Disorder
Definition
Etiology
Pathophysiology
Diagnosis
Treatment
Achalasia
Failure of smooth muscle relaxation at LES Increased LES pressure
Progressive loss of peristaltic function
Usually idiopathic
2o or pseudo-achalasia: e.g. malignancy, Chagas disease (Trypanosoma cruzi)
Inflammatory degeneration of Auerbach’s plexus → increase in LES pressure, incomplete relaxation of LES with swallowing, aperistalsis
CXR: no air in stomach, dilated esophagus Barium studies: esophagus terminates in narrowingatLES(“bird’sbeak”) Endoscopy: normal mucosa
Manometry: definitive diagnosis (signs listed above)
Dilatation of LES with balloon, ± GERD prophylaxis, 50% good response, can repeat, risk of perforation (5%)
Injection of botulinum toxin into LES (temporary)
POEM (perioral endoscopicmyotomy)
Scleroderma
See Rheumatology, RH13
Systemic disease characterized
by vasculopathy and tissue fibrosis (especially skin thickening)
Involves autoimmune, genetic, hormonal, and environmental factors
Dysphagia: caused by reflux, dysmotility, or both
Blood vessel damage → intramural neuronal dysfunction → distal esophageal muscle weakening → aperistalsis and loss of LES tone → reflux → stricture → dysphagia
Clinical features of scleroderma Manometry: decreased pressure in LES, decreasedperistalsisinbodyofesophagus
Medical: aggressive GERD therapy (PPIs bid)
Surgery: anti-reflux surgery (gastroplasty, last resort)
Diffuse Esophageal Spasm
Normal peristalsis interspersed with frequent, repetitive, spontaneous, high pressure, non-peristaltic waves (tertiary peristalsis)
Idiopathic
Potential mechanisms include impaired inhibitory innervation to esophageal body, malfunction in endogenous nitric oxide synthesis
Barium x-ray: “Corkscrew pattern” Manometry: >30% (but <100%) of esophagealcontractionsareaperistaltic Endoscopy: normal mucosa
Reassurance not cardiac pain
Medical: nitrates, calcium channel blockers, anticholinergics have variable benefit
Surgical: long esophageal myotomy if unresponsive to above treatment (rarely helpful); balloon dilatation