Page 362 - TNFlipTest
P. 362
G12 Gastroenterology
Stomach and Duodenum Toronto Notes 2019
• duodenalulcers:6classicalfeatures,buthistoryalonecannotdistinguishfromfunctionaldyspepsia ■ epigastric pain; may localize to tip of xiphoid
■ burning
■ develops 1-3 h after meals
■ relieved by eating and antacids
■ interrupts sleep
■ periodicity (tends to occur in clusters over wk with subsequent periods of remission)
• gastriculcers:moreatypicalsymptoms;abiopsyisnecessarytoexcludemalignancy
Investigations
• endoscopy(mostaccurate)
• upperGIseries
• H. pylori tests (see Table 7)
• fastingserumgastrinmeasurementifZollinger-Ellisonsyndromesuspected(butmostcommoncause
of elevated serum gastrin level is atrophic gastritis)
Treatment
• specificmanagementdependsonetiology;(seeH.pylori,G13,NSAID-InducedUlceration,G13and Stress-Induced Ulceration, G14)
• eradicateH.pyloriifpresent;chiefadvantageoftripletherapyoverPPIistolowerulcerrecurrencerate
• stopNSAIDsifpossible
• startPPI:inhibitsparietalcellH+/K+-ATPasepumpwhichsecretesacid
■ heals most ulcers, even if NSAIDs are continued
• othermedications(e.g.histamineH2-antagonists)lesseffective
• discontinuecigarettesmoking
• nodietmodificationsrequiredbutsomepeoplehavefewersymptomsiftheyavoidcaffeine,alcohol,
and spices
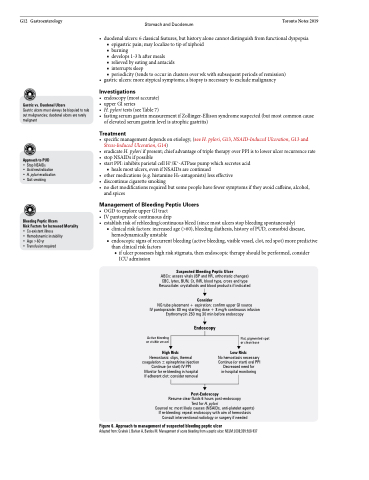
Management of Bleeding Peptic Ulcers
• OGDtoexploreupperGItract
• IVpantoprazolecontinuousdrip
• establishriskofrebleeding/continuousbleed(sincemostulcersstopbleedingspontaneously)
■ clinical risk factors: increased age (>60), bleeding diathesis, history of PUD, comorbid disease, hemodynamically unstable
■ endoscopic signs of recurrent bleeding (active bleeding, visible vessel, clot, red spot) more predictive than clinical risk factors
◆ if ulcer possesses high risk stigmata, then endoscopic therapy should be performed, consider ICU admission
Suspected Bleeding Peptic Ulcer
ABCs: assess vitals (BP and HR, orthostatic changes) CBC, lytes, BUN, Cr, INR, blood type, cross and type Resuscitate: crystalloids and blood products if indicated
Consider
NG tube placement + aspiration: confirm upper GI source
IV pantoprazole: 80 mg starting dose + 8 mg/h continuous infusion Erythromycin 250 mg 30 min before endoscopy
Gastric vs. Duodenal Ulcers
Gastric ulcers must always be biopsied to rule out malignancies; duodenal ulcers are rarely malignant
Approach to PUD
• Stop NSAIDs
• Acid neutralization • H. pylori eradication • Quit smoking
Bleeding Peptic Ulcers
Risk Factors for Increased Mortality • Co-existent illness
• Hemodynamic instability
• Age >60 yr
• Transfusion required
Endoscopy
Active bleeding or visible vessel
High Risk:
Flat, pigmented spot or clean base
Low Risk:
No hemostasis necessary Continue (or start) oral PPI Decreased need for in-hospital monitoring
Hemostasis: clips, thermal coagulation ± epinephrine injection Continue (or start) IV PPI Monitor for re-bleeding in hospital If adherent clot: consider removal
Post-Endoscopy
Resume clear fluids 6 hours post-endoscopy
Test for H. pylori
Counsel re: most likely causes (NSAIDs, anti-platelet agents) If re-bleeding: repeat endoscopy with aim of hemostasis Consult interventional radiology or surgery if needed
Figure 6. Approach to management of suspected bleeding peptic ulcer
Adapted from: Gralnek I, Barkun A, Bardou M. Management of acute bleeding from a peptic ulcer. NEJM 2008;359:928-937