Page 390 - TNFlipTest
P. 390
G40 Gastroenterology
Biliary Tract Toronto Notes 2019
Complication: Primary/Spontaneous Bacterial Peritonitis
• primary/spontaneousbacterialperitonitis(SBP)
■ complicates ascites, but does not cause it (occurs in 10% of cirrhotic ascites); higher risk in patients
with GI bleed
■ 1/3 of patients are asymptomatic, thus do not hesitate to do a diagnostic paracentesis in ascites even
if no clinical indication of infection
■ fever, chills, abdominal pain, ileus, hypotension, worsening encephalopathy, acute kidney injury ■ Gram-negatives compose 70% of pathogens: E. coli (most common), Streptococcus, Klebsiella
• diagnosis
■ absolute neutrophil count in peritoneal fluid >0.25x109 cells/L (250 cells/mm3) ■ Gramstainpositiveinonly10-50%ofpatients
■ culture positive in <80% of patients (not needed for diagnosis)
• prophylaxis:considerinpatientswith:
■ cirrhosis or GI bleed: ceftriaxone IV daily or norfloxacin bid x 7 d
■ previous episode of SBP: long-term prophylaxis with daily norfloxacin or TMP-SMX
• treatment
■ IV antibiotics (cefotaxime 2 g IV q8h or ceftriaxone 2 g IV daily is the treatment of choice for 5 d;
modify if response inadequate or culture shows resistant organisms)
■ IV albumin (1.5 g/kg at time of diagnosis and 1 g/kg on day 3) decreases mortality by lowering risk
of acute renal failure
Biliary Tract
Jaundice
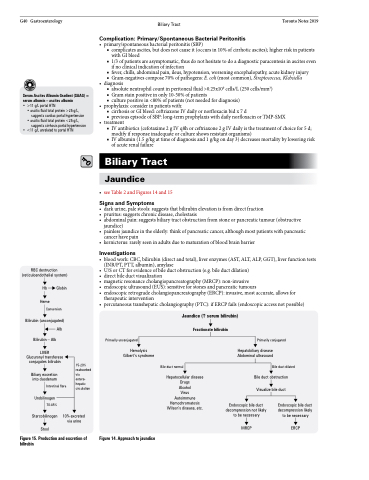
• seeTable2andFigures14and15
Signs and Symptoms
• darkurine,palestools:suggeststhatbilirubinelevationisfromdirectfraction
• pruritus:suggestschronicdisease,cholestasis
• abdominalpain:suggestsbiliarytractobstructionfromstoneorpancreatictumour(obstructive
jaundice)
• painlessjaundiceintheelderly:thinkofpancreaticcancer,althoughmostpatientswithpancreatic
cancer have pain
• kernicterus:rarelyseeninadultsduetomaturationofbloodbrainbarrier
Investigations
• bloodwork:CBC,bilirubin(directandtotal),liverenzymes(AST,ALT,ALP,GGT),liverfunctiontests
Serum Ascites Albumin Gradient (SAAG) = serum albumin – ascites albumin
• >11 g/L portal HTN
• ascitic fluid total protein >25 g/L, suggests cardiac portal hypertension
• ascitic fluid total protein <25 g/L, suggests cirrhosis portal hypertension
• <11 g/L unrelated to portal HTN
RBC destruction (reticuloendothelial system)
Hb Globin
Heme Conversion
Bilirubin (unconjugated) Alb
Bilirubin – Alb
LIVER Glucuronyl transferase conjugates bilirubin
Biliary excretion into duodenum
Intestinal flora
Urobilinogen 70-85%
Stercobilinogen Stool
• • • • •
•
(INR/PT, PTT, albumin), amylase
U/S or CT for evidence of bile duct obstruction (e.g. bile duct dilation) directbileductvisualization magneticresonancecholangiopancreatography(MRCP):non-invasive endoscopicultrasound(EUS):sensitiveforstonesandpancreatictumours endoscopicretrogradecholangiopancreatography(ERCP):invasive,mostaccurate,allowsfor therapeutic intervention percutaneoustranshepaticcholangiography(PTC):ifERCPfails(endoscopicaccessnotpossible)
Jaundice (serum bilirubin)
Fractionate bilirubin
Primarily unconjugated
Hemolysis Gilbert’s syndrome
Primarily conjugated
Hepatobiliary disease Abdominal ultrasound
Bile duct dilated Bile duct obstruction
Visualize bile duct
15-20% reabsorbed via
entero- hepatic circulation
Bile duct normal
Hepatocellular disease Drugs
Alcohol
Virus Autoimmune Hemochromatosis Wilson’s disease, etc.
10% excreted via urine
Endoscopic bile duct decompression not likely to be necessary
MRCP
Endoscopic bile duct decompression likely to be necessary
ERCP
Figure 15. Production and excretion of bilirubin
Figure 14. Approach to jaundice