Page 395 - TNFlipTest
P. 395
Toronto Notes 2019
Pancreas
Gastroenterology G45
Classification
• interstitialedematousvs.necrotizing • mild, moderate, severe
Prognosis
• usuallyabenign,self-limitingcourse,singleorrecurrent • occasionallysevereleadingto:
■ shock
■ pulmonary edema
■ multi-organ dysfunction syndrome
■ GI ulceration due to stress
■ death
■ numerous scales to describe severity: probably most useful is proportion of pancreas not taking up
contrast on CT done 48 h after presentation (necrotic pancreas does not take up the contrast dye) ■ presence of organ failure, particularly organ failure that persists >48 h, is associated with worse
outcomes
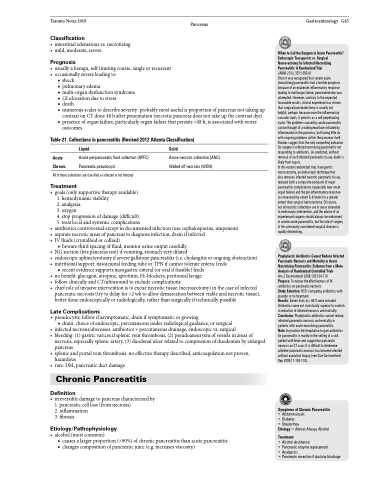
Table 21. Collections in pancreatitis (Revised 2012 Atlanta Classification)
When to Call the Surgeon in Acute Pancreatitis? Endoscopic Transgastric vs. Surgical Necrosectomy for Infected Necrotizing Pancreatitis: A Randomized Trial
JAMA 2012; 307:1053-61
Once it was recognized that severe acute (necrotizing) pancreatitis had a terrible prognosis because of an exuberant inflammatory response leading to multiorgan failure, pancreatectomy was attempted. However, contrary to the expected favourable results, clinical experience has shown that surgical pancreatectomy is usually not
helpful, perhaps because once the inflammatory cascade starts, it persists as a self-perpetuating cycle. The problems caused by acute pancreatitis can be thought of a widespread burn initiated by inflammation in the pancreas, but having little do with ongoing problems within the pancreas itself. Studies suggest that the only compelling indication for surgery is infected necrotizing pancreatitis not responding to antibiotics. As predicted, without removal of such infected pancreatic tissue, death is likely from sepsis.
In this recent randomized trial, transgastric necrosectomy, an endoscopic technique that
also removes infected necrotic pancreatic tissue, reduced both a composite end-point of major pancreatitis complications (especially new onset organ failure) and the pro-inflammatory response (as measured by serum IL-6 levels) to a greater extent than surgical necrosectomy. Of course,
not all necrotic collections are in areas amenable to endoscopic intervention, and the advice of an experienced surgeon should always be welcomed in severe acute pancreatitis, but the role of surgery in this previously considered surgical disease is rapidly diminishing.
Prophylactic Antibiotics Cannot Reduce Infected Pancreatic Necrosis and Mortality in Acute Necrotizing Pancreatitis: Evidence from a Meta- Analysis of Randomized Controlled Trials
Am J Gastroenterol 2008;103:104-110
Purpose: To review the effectiveness of IV antibiotics on pancreatic necrosis.
Study Selection: RCTs comparing antibiotics with placebo or no treatment.
Results: Seven trials (n=467) were included. Antibiotics were not statistically superior to controls in reduction of infected necrosis and mortality. Conclusion: Prophylactic antibiotics cannot reduce infected pancreatic necrosis and mortality in patients with acute necrotizing pancreatitis.
Note: In practice the temptation to give antibiotics for pancreatitis is mainly in the setting of a sick patient with fever and suggestive pancreatic necrosis on CT scan. It is difficult to determine whether pancreatic necrosis has become infected without aspiration biopsy (see Curr Gastroenterol Rep 2009;11:104-110).
Symptoms of Chronic Pancreatitis
• Abdominal pain
• Diabetes
• Steatorrhea
Etiology = Almost Always Alcohol
Treatment
• Alcohol abstinence
• Pancreatic enzyme replacement • Analgesics
Acute Chronic
Liquid
Acute peripancreatic fluid collection (APFC) Pancreatic pseudocyst
Solid
Acute necrotic collection (ANC) Walled-off necrosis (WON)
All of these collections are classified as infected or not infected
Treatment
• goals(onlysupportivetherapyavailable) 1. hemodynamic stability
2. analgesia
3. oxygen
4. stop progression of damage (difficult)
5. treat local and systemic complications
• antibioticscontroversialexceptindocumentedinfection(usecephalosporins,imipenem)
• aspiratenecroticareasofpancreastodiagnoseinfection;drainifinfected
• IVfluids(crystalloidorcolloid)
■ beware third spacing of fluid, monitor urine output carefully
• NGsuction(letspancreasrest)ifvomiting,stomachverydilated
• endoscopicsphincterotomyifseveregallstonepancreatitis(i.e.cholangitisorongoingobstruction)
• nutritionalsupport:nasojejunalfeedingtubeorTPNifcannottolerateentericfeeds
■ recent evidence supports nasogastric enteral (or oral if feasible) feeds
• no benefit: glucagon, atropine, aprotinin, H2-blockers, peritoneal lavage
• followclinicallyandCT/ultrasoundtoexcludecomplications
• chiefroleofinvasiveinterventionistoexcisenecrotictissue(necrosectomy)inthecaseofinfected
pancreatic necrosis (try to delay for >2 wk to allow demarcation between viable and necrotic tissue), better done endoscopically or radiologically, rather than surgically if technically possible
Late Complications
• pseudocysts:followifasymptomatic,drainifsymptomaticorgrowing
■ drain: choice of endoscopic, percutaneous under radiological guidance, or surgical
• infectednecrosis/abscesses:antibiotics+percutaneousdrainage,endoscopicvs.surgical
• bleeding: (1) gastric varices if splenic vein thrombosis, (2) pseudoaneurysm of vessels in areas of
necrosis, especially splenic artery, (3) duodenal ulcer related to compression of duodenum by enlarged
pancreas
• splenicandportalveinthrombosis:noeffectivetherapydescribed,anticoagulationnotproven,
hazardous
• rare:DM,pancreaticductdamage
Chronic Pancreatitis
Definition
• irreversibledamagetopancreascharacterizedby 1. pancreatic cell loss (from necrosis)
2. inflammation
3. fibrosis
Etiology/Pathophysiology
• alcohol(mostcommon)
■ causes a larger proportion (>90%) of chronic pancreatitis than acute pancreatitis ■ changes composition of pancreatic juice (e.g. increases viscosity)
• Pancreatic resection if ductular blockage