Page 474 - TNFlipTest
P. 474
GM6 Geriatric Medicine
Differential Diagnoses of Common Presentations
Toronto Notes 2019
Common Causes of Constipation in the Geriatric Population include:
• Primary impaired colonic and anorectal
function
• Drugs (see below)
• Diet (dehydration, low fibre “tea and toast”
diet)
• Colo-anorectal disorders (cancer, masses,
stenosis, strictures)
• Neurologic (stroke, dementia, Parkinson’s,
autonomic neuropathy)
• Psychiatric (depression, anxiety
Drugs Associated with Constipation include:
• OTC (antihistamines, NSAIDs)
• Opioids
• Psychotropic (antipsychotics, TCAs) • Anticholinergics
• Calcium channel blockers
• Diuretics
• Supplements (iron or calcium) Diagnostic approach to chronic constipation in adults. Am Fam Physician 2011;84:299-306
Treatment of Constipation in Older Adults
CMAJ 2013;185(8):663-70
Objectives: To discuss management of constipation in older adults.
Results/Conclusions: In older adults, the predominant symptom of constipation is more frequently straining than decreased stool frequency. RCTs support the use of osmotic agents to treat symptoms of constipation in older adults. In contrast evidence supporting the use of bulk agents, stool softeners stimulants and prokinetic agents is lacking, limited and inconsistent.
Constipation
• seeGastroenterology,G24 Definition
• RomeIIIDiagnosticCriteria:<3bowelmovementsinonewkand/orhardstools,straining,senseof blockade, needing manual maneuvers or incomplete evacuation on more than 25% of occasions for at least 12 wk (does not need to be consecutive). Symptoms must have occurred in the last 3 mo, with symptom onset ≥6 mo before diagnosis can be made
Epidemiology
• chronicconstipationincreaseswithage(upto1/3ofpatients>65yrexperienceconstipationand1/2of patients >80 yr)
• intheelderly,chronicconstipationmaypresentasfecalimpaction
Pathophysiology
• impairedrectalsensation(increasedrectaldistentionrequiredtostimulatetheurgetodefecate) • colorectaldysmotility
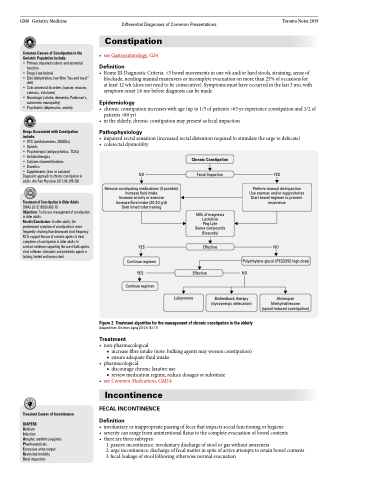
NO
Remove constipating medications (if possible) Increase fluid intake
Increase activity or exercise Increase fibre intake (20-30 g/d)
Start timed toilet training
YES
Continue regimen YES
Continue regimen
Chronic Constipation
Fecal Impaction
Milk of magnesia Lactulose Peg-Lyte Senna compounds Bisacodyl
Effective
YES
Perform manual disimpaction Use enemas and/or suppositories Start bowel regimen to prevent recurrence
NO
Polyethylene glycol (PEG3350 high dose) NO
Effective
Lubiprotone
Biofeedback therapy (dyssynergic defecation)
Alvimopan Methylnaltrexone (opioid-induced constipation)
Transient Causes of Incontinence
DIAPERS
Delirium
Infection
Atrophic urethritis/vaginitis Pharmaceuticals Excessive urine output Restricted mobility
Stool impaction
Figure 2. Treatment algorithm for the management of chronic constipation in the elderly
Adapted from: Clin Interv Aging 2010;5:163-171
Treatment
• non-pharmacological
■ increase fibre intake (note: bulking agents may worsen constipation) ■ ensure adequate fluid intake
• pharmacological
■ discourage chronic laxative use
■ review medication regime, reduce dosages or substitute
• seeCommonMedications,GM14
Incontinence
FECAL INCONTINENCE
Definition
• involuntaryorinappropriatepassingoffecesthatimpactssocialfunctioningorhygiene
• severitycanrangefromunintentionalflatustothecompleteevacuationofbowelcontents • there are three subtypes:
1. passive incontinence: involuntary discharge of stool or gas without awareness
2. urge incontinence: discharge of fecal matter in spite of active attempts to retain bowel contents 3. fecal: leakage of stool following otherwise normal evacuation