Page 619 - TNFlipTest
P. 619
Toronto Notes 2019 CNS Infections
Prevention
• seePediatrics,P55
• immunization
■ children: immunization against H. influenzae type B (Pentacel®), S. pneumoniae (Synflorix®, Prevnar-13®), N. meningitidis (Menjugate®, Menactra®, Nimenrix®, Menveo®, Bexsero®)
■ adults: immunization against N. meningitidis in selected circumstances (outbreaks, travel, epidemics) and S. pneumoniae (Pneumovax®) for high-risk groups
• prophylaxis:closecontactsofpatientsinfectedwithH.influenzaetypeBshouldbetreatedwith rifampin if they live with an inadequately immunized (<4 yr) or immunocompromised child (<18 yr); ciprofloxacin, rifampin, or ceftriaxone if close or household contact of a patient with N. meningitidis; meningococcal vaccines are also recommended for post-exposure prophylaxis for close contacts and in outbreak control
Prognosis
• complications
■ death, headache, seizures, cerebral edema, hydrocephalus, SIADH, residual neurological deficit
(especially CN VIII), deafness • mortality
■ S. pneumoniae 25%; N. meningitidis 5-10%; H. influenzae 5%
■ worse prognosis if: extremes of age, delays in diagnosis and treatment, stupor or coma, seizures,
focal neurological signs, septic shock at presentation
Encephalitis
Definition
• inflammationofthebrainparenchyma
Etiology
• identifiedinonly40-70%ofcases
■ when cause is identified, the most common etiology is viral: HSV, VZV, EBV, CMV, enteroviruses,
parechoviruses, West Nile and other arboviruses, influenza and other respiratory viruses, HIV,
mumps, measles, rabies, polio
■ bacteria: L. monocytogenes, mycobacteria, spirochetes (Lyme, syphillis), Mycoplasma pneumoniae
■ parasites: protozoa (e.g. Toxoplasma) and helminths (rare)
■ fungi: e.g. Cryptococcus
■ post-infectious (e.g. acute disseminated encephalomyelitis [ADEM])
■ auto-antibody mediated encephalitis
◆ anti-N-methyl-D-aspartate (NMDA) receptor encephalitis most common
◆ in adults, most autoantibody-mediated encephalitis cases are associated with malignancy
Pathophysiology
• acuteinflammatorydiseaseofthebrainduetodirectinvasionorpathogen-initiatedimmuneresponse • virusesmayreachtheCNSviaperipheralnerves(e.g.rabies,HSV)
• herpessimplexencephalitis
■ acute, necrotizing, asymmetrical hemorrhagic process with lymphocytic and plasma cell reaction which usually involves the medial temporal and inferior frontal lobes
■ associated with HSV-1, less likely caused by HSV-2
• influenzaandotherrespiratoryvirusesareassociatedwithacutenecrotizingencephalopathy(ANE);
likely mediated by pathogen-initiated immune response
Clinical Presentation
• constitutional: fever, chills, malaise, nausea/vomiting
• meningealinvolvement(meningoencephalitis):headache,nuchalrigidity
• parenchymalinvolvement:seizures,alteredmentalstatus,focalneurologicalsigns • herpessimplexencephalitis
■ acute onset (<1 wk) of focal neurological signs: hemiparesis, ataxia, aphasia, focal or generalized seizures
■ temporal lobe involvement: behavioural disturbance
■ usually rapidly progressive over several days and may result in coma or death
■ common sequelae: memory and behavioural disturbances
■ rare complication: development of encephalopathy and Kluver-Bucy syndrome characteristics one
month after completion of treatment for HSV encephalopathy
Investigations
• CSF:openingpressure,cellcountanddifferential,glucose,protein,Gramstain,bacterialC&S,PCRfor HSV, VZV, EBV, enteroviruses/parechoviruses, M. pneumoniae, and selectively for other less common etiologies
• serology:mayaiddiagnosisofcertaincausesofencephalitis(e.g.EBV,WestNilevirus,rabies, Bartonella henselae)
• imaging/neurologic studies: CT, MRI, EEG to define anatomical sites affected
• invasivetesting:braintissuebiopsymayberequiredforculture,histologicalexamination,and
immunocytochemistry (if diagnosis not clear via non-invasive means)
• findingsinherpessimplexencephalitis(mustruleoutduetohighmortality)
■ CT/MRI: medial temporal lobe necrosis
■ EEG: early focal slowing, periodic discharges
Infectious Diseases ID19
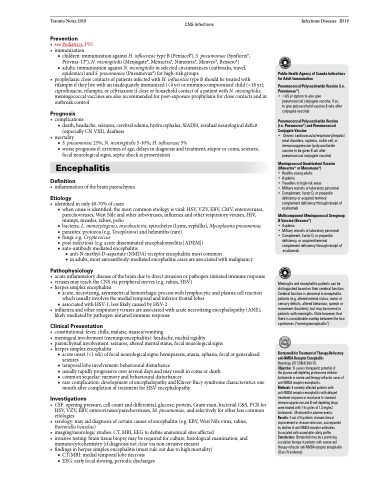
Public Health Agency of Canada Indications for Adult Immunization
Pneumococcal Polysaccharide Vaccine (i.e. Pneumovax®)
• >65 yr (option to also give
pneumococcal conjugate vaccine; if so, to give polysaccharid vaccine 8 wks after conjugate vaccine)
Pneumococcal Polysaccharide Vaccine (i.e. Pneumovax®) and Pneumococcal Conjugate Vaccine
• Chroniccardiovascular/respiratory/hepatic/
renal disorders, asplenia, sickle cell, or immunosuppression (polysaccharide vaccine to be given 8 wk after pneumococcal conjugate vaccine)
Meningococcal Quadrivalent Vaccine (Menactra® or Menomune®)
• Healthy young adults
• Asplenia
• Travellers to high-risk areas
• Military recruits or laboratory personnel
• Complement, factor D, or properdin
deficiency or acquired terminal complement deficiency through receipt of eculizumab
Multicomponent Meningococcal Serogroup B Vaccine (Bexsero®)
• Asplenia
• Military recruits or laboratory personnel
• Complement, factor D, or properdin deficiency, or acquired terminal complement deficiency through receipt of
eculizumab
Meningitis and encephalitis patients can be distinguished based on their cerebral function. Cerebral function is abnormal in encephalitis patients (e.g. altered mental status, motor or sensory deficits, altered behaviour, speech or movement disorders), but may be normal in patients with meningitis. Note however, that there is considerable overlap between the two syndromes (“meningoencephalitis”)
Bortezomib for Treatment of Therapy-Refractory anti-NMDA Receptor Encephalitis
Neurology 2017;88(4):366-70.
Objective: To assess therapeutic potential of
the plasma-cell-depleting proteasome inhibitor bortezomib in severe and therapy-refractor cases of anti-NMDA receptor encephalitis.
Methods: 5 severely affected patients with anti-NMDA receptor encephalitis with delayed treatment response or resistance to standard immunosuppressive and B-cell-depleting drugs were treated with 1-6 cycles of 1.3 mg/m2 bortezomib. Monitoredforadverseevents. Results: 4 out of 5 patients showed clinical improvement or disease remission, accompanied by decline of anti-NMDA receptor antibodies. Associated with acceptable safety profile. Conclusions: Bortezomib may be a promising escalation therapy in patients with severe and therapy-refractor anti-NMDA receptor encephalitis (Class IV evidence).