Page 719 - TNFlipTest
P. 719
Toronto Notes 2019
Acute Kidney Injury
Nephrology NP19
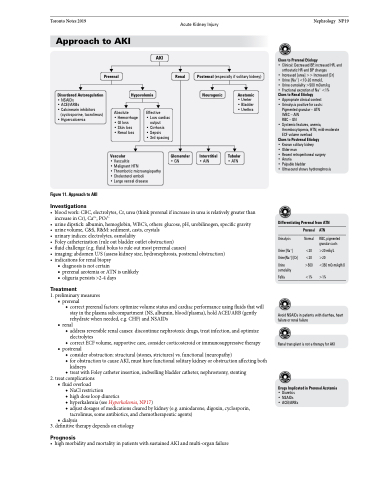
Approach to AKI
Prerenal
Absolute
• Hemorrhage • GI loss
• Skin loss
• Renal loss
Vascular
AKI
Effective
• Low cardiac
output
• Cirrhosis
• Sepsis
• 3rd spacing
Renal
Postrenal (especially if solitary kidney)
Clues to Prerenal Etiology
• Clinical: Decreased BP, increased HR, and orthostatic HR and BP changes
• Increased [urea] >> Increased [Cr]
• Urine [Na+] <10-20 mmol/L
• Urine osmolality >500 mOsm/kg
• Fractional excretion of Na+ <1% Clues to Renal Etiology
• Appropriate clinical context • Urinalysis positive for casts: Pigmented granular – ATN
WBC – AIN
RBC–GN
• Systemic features, anemia,
thrombocytopenia, HTN, mild-moderate
ECF volume overload
Clues to Postrenal Etiology
• Known solitary kidney
• Older man
• Recent retroperitoneal surgery
• Anuria
• Palpable bladder
• Ultrasound shows hydronephrosis
Differentiating Prerenal from ATN
Disordered Autoregulation
• NSAIDs
• ACEI/ARBs
• Calcineurin inhibitors
(cyclosporine, tacrolimus) • Hypercalcemia
Hypovolemia
Neurogenic
Interstitial
• AIN
Anatomic
• Ureter • Bladder • Urethra
Tubular
• ATN
Figure 11. Approach to AKI
Investigations
• Vasculitis
• Malignant HTN
• Thrombotic microangiopathy • Cholesterol emboli
• Large vessel disease
Glomerular
• GN
• bloodwork:CBC,electrolytes,Cr,urea(thinkprerenalifincreaseinureaisrelativelygreaterthan increase in Cr), Ca2+, PO43-
• urinedipstick:albumin,hemoglobin,WBC’s,others:glucose,pH,urobilinogen,specificgravity
• urine volume, C&S, R&M: sediment, casts, crystals
• urinaryindices:electrolytes,osmolality
• Foleycatheterization(ruleoutbladderoutletobstruction)
• fluidchallenge(e.g.fluidbolustoruleoutmostprerenalcauses)
• imaging:abdomenU/S(assesskidneysize,hydronephrosis,postrenalobstruction)
• indicationsforrenalbiopsy
■ diagnosis is not certain
■ prerenal azotemia or ATN is unlikely ■ oliguria persists >2-4 days
Treatment
1. preliminary measures ■ prerenal
◆ correct prerenal factors: optimize volume status and cardiac performance using fluids that will stay in the plasma subcompartment (NS, albumin, blood/plasma), hold ACEI/ARB (gently rehydrate when needed, e.g. CHF) and NSAIDs
■ renal
◆ address reversible renal causes: discontinue nephrotoxic drugs, treat infection, and optimize
electrolytes
◆ correct ECF volume, supportive care, consider corticosteroid or immunosuppressive therapy
■ postrenal
◆ consider obstruction: structural (stones, strictures) vs. functional (neuropathy)
◆ for obstruction to cause AKI, must have functional solitary kidney or obstruction affecting both
kidneys
◆ treat with Foley catheter insertion, indwelling bladder catheter, nephrostomy, stenting
2. treat complications ■ fluid overload
◆ NaCl restriction
◆ high dose loop diuretics
◆ hyperkalemia (see Hyperkalemia, NP17)
◆ adjust dosages of medications cleared by kidney (e.g. amiodarone, digoxin, cyclosporin,
tacrolimus, some antibiotics, and chemotherapeutic agents) ■ dialysis
3. definitive therapy depends on etiology
Prognosis
• highmorbidityandmortalityinpatientswithsustainedAKIandmulti-organfailure
Urinalysis
Urine [Na+] Urine[Na+]/[Cr]
Urine osmolality
FeNa
Prerenal ATN
Normal RBC, pigmented granular casts
<20 >20 mEq/L <20 >20
>500 <350 mOsm/kgH2O <1% >1%
Avoid NSAIDs in patients with diarrhea, heart failure or renal failure
Renal transplant is not a therapy for AKI
Drugs Implicated in Prerenal Azotemia
• Diuretics • NSAIDs
• ACEI/ARBs