Page 751 - TNFlipTest
P. 751
Toronto Notes 2019 Lumbar Puncture Neurology N9 Lumbar Puncture
Indications
• diagnostic:CNSinfection(meningitis,encephalitis),inflammatorydisorder(MS,Guillain-Barré, vasculitis), subarachnoid hemorrhage (if CT negative), CNS neoplasm (neoplastic meningitis)
• therapeutic:toadministeranesthesia,chemotherapy,contrastmedia ■ to decrease ICP (pseudotumour cerebri, NPH)
Contraindications
• masslesioncausingincreasedICP,couldleadtocerebralherniation;CTfirstifsuspectmasslesion • infectionoverLPsite/suspectedepiduralabscess
• lowplatelets(<50,000)ortreatmentwithanticoagulation(highINRoraPTT)
• uncooperativepatient
Complications
• tonsillarherniation(rare)
• SDH(rare)
• transient6thnervepalsy(rare)
• post-LPheadache(5-40%):worsewhenupright,bettersupine;generallyonsetwithin24h
■ prevention: smaller gauge (i.e. 22) needle, reinsert stylet prior to needle removal, blunt-ended needle ■ symptomatic treatment: caffeine and sodium benzoate injection
■ corrective treatment: blood patch (autologous)
• spinalepiduralhematoma • infection
LP Tubes
• tube#1:cellcountanddifferential:RBCs,WBCs,anddifferential
■ xanthochromia (yellow bilirubin pigmentation implies recent bleed into CSF, diagnostic of SAH)
• tube#2:chemistry:glucose(comparetoserumglucose)andprotein
• tube#3:microbiology:GramstainandC&S
■ specific tests depending on clinical situation/suspicion
◆ viral: PCR for herpes simplex virus (HSV) and other viruses
◆ bacterial: polysaccharide antigens of H. influenzae, N. meningitidis, S. pneumoniae ◆ fungal: cryptococcal antigen, culture
◆ TB: acid-fast stain, TB culture, TB PCR
• tube#4:cytology:forevidenceofmalignantcells,ifclinicalsuspicionislowforneoplasm,consider sending tube #4 for cell count
The needle for a LP is inserted into one of L3-4, L4-5, or L5-S1 interspaces
Do not delay antibiotics while waiting for a LP if infection is suspected
RBCs in tube #1>>#5 → traumatic tap RBCs in tube #1=#5 → SAH
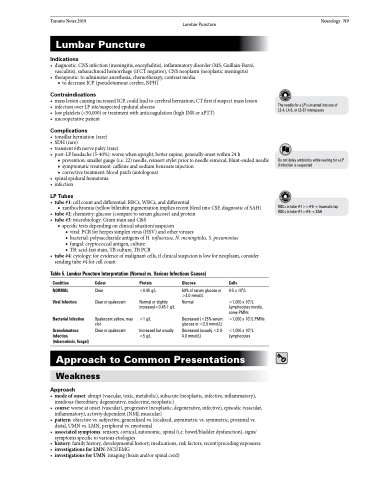
Table 5. Lumbar Puncture Interpretation (Normal vs. Various Infectious Causes)
Condition
NORMAL Viral Infection
Bacterial Infection
Granulomatous Infection (tuberculosis, fungal)
Colour
Clear
Clear or opalescent
Opalescent yellow, may clot
Clear or opalescent
Protein
<0.45 g/L
Normal or slightly increased<0.45-1 g/L
>1 g/L
Increased but usually <5 g/L
Glucose
60% of serum glucose or >3.0 mmol/L
Normal
Decreased (<25% serum glucose or <2.0 mmol/L) Decreased (usually <2.0- 4.0 mmol/L)
Cells
0-5 x 106/L
<1,000 x 106/L Lymphocytes mostly, some PMNs
>1,000 x 106/L PMNs
<1,000 x 106/L Lymphocytes
Approach to Common Presentations
Weakness
Approach
• modeofonset:abrupt(vascular,toxic,metabolic),subacute(neoplastic,infective,inflammatory), insidious (hereditary, degenerative, endocrine, neoplastic)
• course:worseatonset(vascular),progressive(neoplastic,degenerative,infective),episodic(vascular, inflammatory), activity dependent (NMJ, muscular)
• pattern:objectivevs.subjective,generalizedvs.localized,asymmetricvs.symmetric,proximalvs. distal, UMN vs. LMN, peripheral vs. myotomal
• associatedsymptoms:sensory,cortical,autonomic,spinal(i.e.bowel/bladderdysfunction),signs/ symptoms specific to various etiologies
• history:familyhistory,developmentalhistory,medications,riskfactors,recent/precedingexposures
• investigationsforLMN:NCS/EMG
• investigationsforUMN:imaging(brainand/orspinalcord)