Page 963 - TNFlipTest
P. 963
Toronto Notes 2019 Hip
POSTERIOR HIP DISLOCATION
• mostfrequenttypeofhipdislocation
• mechanism:severeforcetokneewithhipflexedandadducted
■ e.g. knee into dashboard in MVC
• clinicalfeatures:shortened,adducted,internallyrotatedlimb • treatment
■ closed reduction under conscious sedation/GA only if no associated femoral neck fracture or ipsilateral displacement
Orthopedics OR29
■ ORIF if unstable, intra-articular fragments, or posterior wall fracture
■ post-reduction CT to assess joint congruity and fractures
■ if reduction is unstable, put in traction x 4-6 wk
COMPLICATIONS FOR ALL HIP DISLOCATIONS
Rochester Method to Reduce Posterior Dislocations
• Patient lying supine with hip and knee
flexed on injured side
• Surgeon stands on patient’s injured side
• Surgeon passes one arm under patient’s
flexed knee, reaching to place that hand on patient’s other knee (thus supporting patient’s injured leg)
• With other hand, surgeon grasps patient’s ankle on injured side, applying traction, while assistant stabilizes pelvis
• Reduction via traction, internal rotation, then external rotation once femoral head clears acetabular rim
X-Ray Features of Subcapital Hip Fractures
• Disruption of Shenton’s line (a radiographic line drawn along the upper margin of the obturator foramen, extending along the inferomedial side of the femoral neck)
• Altered neck-shaft angle (normal is 120- 130°)
DVT Prophylaxis in Hip Fractures
LMWH (i.e. enoxaparin 40 mg SC bid), fondaparinux, low dose heparin on admission, do not give <12 h before surgery
AVN of Femoral Head
• Distal to proximal blood supply along femoral neck to head (medial and lateral femoral circumflex arteries)
• Susceptible to AVN if blood supply disrupted
• Etiology: femoral neck fracture, chronic systemic steroid use, SCFE, Legg-Calvé- Perthes, SLE, RA
Comparative Effectiveness of Pain Management Interventions for Hip Fracture: A Systematic Review
Study: Randomized controlled trials (RCTs); nonrandomized controlled trials (non-RCTs); and cohort studies of pain management techniques in older adults after acute hip fracture.
Conclusions: Nerve blockade seems to be effective in reducing acute pain after hip fracture. Low-level evidence suggests that preoperative traction does not reduce acute pain. Evidence was insufficient on the benefits and harms of many other interventions.
• post-traumaticOA
• AVNoffemoralhead
• fractureoffemoralhead,neck,orshaft
• sciaticnervepalsyin25%(10%permanent) • HO
• thromboembolism–DVT/PE
Hip Fracture
General Features
• acuteonsetofhippain
• unabletoweight-bear
• shortenedandexternally-rotatedleg • painfulROM
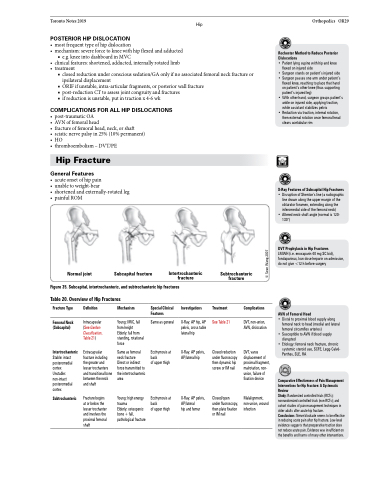
Normal joint
Subcapital fracture
Intertrochanteric fracture
Subtrochanteric fracture
Figure 35. Subcapital, intertrochanteric, and subtrochanteric hip fractures Table 20. Overview of Hip Fractures
Fracture Type
Femoral Neck (Subcapital)
Intertrochanteric
Stable: intact posteromedial cortex Unstable: non-intact posteromedial cortex
Subtrochanteric
Definition
Intracapsular (See Garden Classification, Table 21)
Extracapsular fracture including the greater and lesser trochanters and transitional bone between the neck and shaft
Fracture begins at or below the lesser trochanter and involves the proximal femoral shaft
Mechanism
Young: MVC, fall from height Elderly: fall from standing, rotational force
Same as femoral neck fracture
Direct or indirect force transmitted to the intertrochanteric area
Young: high energy trauma
Elderly: osteopenic bone + fall, pathological fracture
Special Clinical Features
Same as general
Ecchymosis at back
of upper thigh
Ecchymosis at back
of upper thigh
Investigations
X-Ray: AP hip, AP pelvis, cross table lateral hip
X-Ray: AP pelvis, AP/lateral hip
X-Ray: AP pelvis, AP/lateral
hip and femur
Treatment
See Table 21
Closed reduction under fluoroscopy then dynamic hip screw or IM nail
Closed/open under fluoroscopy, then plate fixation or IM nail
Complications
DVT, non-union, AVN, dislocation
DVT, varus displacement of proximal fragment, malrotation, non- union, failure of fixation device
Malalignment, non-union, wound infection
© Sean Wang 2007