Page 970 - TNFlipTest
P. 970
OR36 Orthopedics
Patella
Toronto Notes 2019
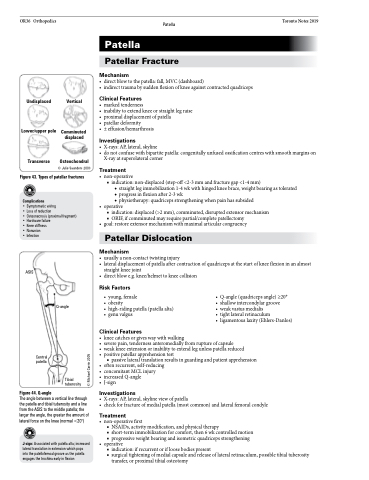
Undisplaced
Lower/upper pole
Transverse
Figure 43. Types of patellar fractures
Complications
• Symptomatic wiring
• Loss of reduction
• Osteonecrosis (proximal fragment) • Hardware failure
• Knee stiffness
• Nonunion
• Infection
Patella
Patellar Fracture
Mechanism
• directblowtothepatella:fall,MVC(dashboard)
• indirecttraumabysuddenflexionofkneeagainstcontractedquadriceps
Clinical Features
• markedtenderness
• inabilitytoextendkneeorstraightlegraise • proximaldisplacementofpatella
• patellardeformity
• ±effusion/hemarthrosis
Investigations
• X-rays: AP, lateral, skyline
• donotconfusewithbipartitepatella:congenitallyunfusedossificationcentreswithsmoothmarginson
X-ray at superolateral corner
Treatment
• non-operative
■ indication: non-displaced (step-off <2-3 mm and fracture gap <1-4 mm)
◆ straight leg immobilization 1-4 wk with hinged knee brace, weight bearing as tolerated ◆ progress in flexion after 2-3 wk
◆ physiotherapy: quadriceps strengthening when pain has subsided
• operative
■ indication: displaced (>2 mm), comminuted, disrupted extensor mechanism ■ ORIF, if comminuted may require partial/complete patellectomy
• goal:restoreextensormechanismwithmaximalarticularcongruency
Patellar Dislocation
Mechanism
• usuallyanon-contacttwistinginjury
• lateraldisplacementofpatellaaftercontractionofquadricepsatthestartofkneeflexioninanalmost
Vertical
Comminuted displaced
Osteochondral
© Julie Saunders 2003
ASIS
straight knee joint
• directblowe.g.knee/helmettokneecollision
Risk Factors
• young, female
• obesity
• high-ridingpatella(patellaalta) • genuvalgus
Clinical Features
Figure 44. Q-angle
Central patella
• kneecatchesorgiveswaywithwalking
• severepain,tendernessanteromediallyfromruptureofcapsule
• weakkneeextensionorinabilitytoextendlegunlesspatellareduced • positivepatellarapprehensiontest
■ passive lateral translation results in guarding and patient apprehension • oftenrecurrent,self-reducing
• concomitantMCLinjury
• increasedQ-angle
• J-sign
Investigations
• X-rays:AP,lateral,skylineviewofpatella
• checkforfractureofmedialpatella(mostcommon)andlateralfemoralcondyle
Treatment
• non-operativefirst
■ NSAIDs, activity modification, and physical therapy
■ short-term immobilization for comfort, then 6 wk controlled motion ■ progressive weight bearing and isometric quadriceps strengthening
• operative
■ indication: if recurrent or if loose bodies present
■ surgical tightening of medial capsule and release of lateral retinaculum, possible tibial tuberosity
transfer, or proximal tibial osteotomy
The angle between a vertical line through the patella and tibial tuberosity and a line from the ASIS to the middle patella; the larger the angle, the greater the amount of lateral force on the knee (normal <20°)
J-sign: Associated with patella alta; increased lateral translation in extension which pops into the patellofemoal groove as the patella engages the trochlea early in flexion
Q-angle
• Q-angle (quadriceps angle) ≥20° • shallow intercondylar groove
• weak vastus medialis
• tight lateral retinaculum
• ligamentouslaxity(Ehlers-Danlos)
Tibial tuberosity
© Michael Corrin 2005