Page 1060 - TNFlipTest
P. 1060
P26 Pediatrics
Endocrinology Toronto Notes 2019
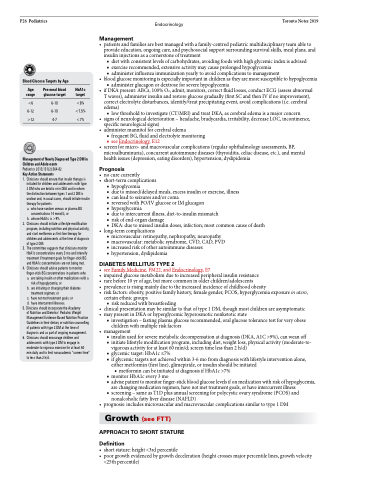
Blood Glucose Targets by Age
Management
• patientsandfamiliesarebestmanagedwithafamily-centredpediatricmultidisciplinaryteamableto provide education, ongoing care, and psychosocial support surrounding survival skills, meal plans, and insulin injections as a cornerstone of treatment
■ diet with consistent levels of carbohydrates, avoiding foods with high glycemic index is advised ■ exercise recommended, extensive activity may cause prolonged hypoglycemia
■ administer influenza immunization yearly to avoid complications to management
• bloodglucosemonitoringisespeciallyimportantinchildrenastheyaremoresusceptibletohypoglycemia ■ administer glucagon or dextrose for severe hypoglycemia
• ifDKApresent:ABCs,100%O2,admit,monitors,correctfluidlosses,conductECG(assessabnormal T waves), administer insulin and restore glucose gradually (first SC and then IV if no improvement), correct electrolyte disturbances, identify/treat precipitating event, avoid complications (i.e. cerebral edema)
■ low threshold to investigate (CT/MRI) and treat DKA, as cerebral edema is a major concern
• signs of neurological deterioration – headache, bradycardia, irritability, decrease LOC, incontinence,
specific neurological signs)
• administermannitolforcerebraledema
■ frequent BG, fluid and electrolyte monitoring
■ see Endocrinology, E12
• screenformicro-andmacrovascularcomplications(regularophthalmologyassessments,BP, microalbuminuria), concurrent autoimmune diseases (thyroiditis, celiac disease, etc.), and mental health issues (depression, eating disorders), hypertension, dyslipidemia
Prognosis
• nocurecurrently
• short-termcomplications
■ hypoglycemia
■ due to missed/delayed meals, excess insulin or exercise, illness
■ can lead to seizures and/or coma
■ reversedwithPO/IVglucoseorIMglucagon
■ hyperglycemia
■ due to intercurrent illness, diet-to-insulin mismatch
■ risk of end-organ damage
■ DKA: due to missed insulin doses, infection; most common cause of death
• long-termcomplications
■ microvascular: retinopathy, nephropathy, neuropathy
■ macrovascular: metabolic syndrome, CVD, CAD, PVD ■ increased risk of other autoimmune diseases
■ hypertension, dyslipidemia
DIABETES MELLITUS TYPE 2
• seeFamilyMedicine,FM22,andEndocrinology,E7
• impairedglucosemetabolismduetoincreasedperipheralinsulinresistance
• rarebefore10yrofage,butmorecommoninolderchildren/adolescents
• prevalenceisrisingmainlyduetotheincreasedincidenceofchildhoodobesity
• risk factors: obesity, positive family history, female gender, PCOS, hyperglycemia exposure in utero,
certain ethnic groups
■ risk reduced with breastfeeding
• clinicalpresentationmaybesimilartothatoftype1DM,thoughmostchildrenareasymptomatic • maypresentinDKAorhyperglycemichyperosmoticnonketoticstate
■ investigation – fasting plasma glucose recommended, oral glucose tolerance test for very obese children with multiple risk factors
• management
■ insulin used for severe metabolic decompensation at diagnosis (DKA, A1C >9%), can wean off
■ initiate lifestyle modification program, including diet, weight loss, physical activity (moderate-to-
vigorous activity for at least 60 min/d; screen time less than 2 h/d)
■ glycemic target: HbA1c ≤7%
■ if glycemic targets not achieved within 3-6 mo from diagnosis with lifestyle intervention alone,
either metformin (first line), glimepiride, or insulin should be initiated ◆ metformin can be initiated at diagnosis if HbA1c >7%
■ monitor HbA1c every 3 mo
■ advisepatienttomonitorfinger-stickbloodglucoselevelsifonmedicationwithriskofhypoglycemia,
are changing medication regimen, have not met treatment goals, or have intercurrent illness
■ screening – same as T1D plus annual screening for polycystic ovary syndrome (PCOS) and
nonalcoholic fatty liver disease (NAFLD)
• prognosis:includesmicrovascularandmacrovascularcomplicationssimilartotype1DM
Growth (see FTT)
APPROACH TO SHORT STATURE
Definition
• shortstature:height<3rdpercentile
• poorgrowthevidencedbygrowthdeceleration(heightcrossesmajorpercentilelines,growthvelocity
Age range
<6 6-12 >12
Pre-meal blood glucose target
6-10 6-10 4-7
HbA1c target
<8% <7.5% <7%
Management of Newly Diagnosed Type 2 DM in Children and Adolescents
Pediatrics 2013;131(2):364-82
Key Action Statements
1. Cliniciansshouldensurethatinsulintherapyis initiated for children and adolescents with type
2 DM who are ketotic or in DKA and in whom the distinction between types 1 and 2 DM is unclear and, in usual cases, should initiate insulin therapy for patients
a. who have random venous or plasma BG concentrations 14 mmol/L; or
b. whoseHbA1cis>9%.
2. Cliniciansshouldinitiatealifestylemodification
program, including nutrition and physical activity, and start metformin as first-line therapy for children and adolescents at the time of diagnosis of type 2 DM.
3. The committee suggests that clinicians monitor HbA1c concentrations every 3 mo and intensify treatment if treatment goals for finger-stick BG and HbA1c concentrations are not being met.
4. Cliniciansshouldadvisepatientstomonitor finger-stick BG concentrations in patients who
a. aretakinginsulinorothermedicationswitha
risk of hypoglycemia; or
b. areinitiatingorchangingtheirdiabetes
treatment regimen; or
c. have not met treatment goals; or
d. have intercurrent illnesses.
5. Clinicians should incorporate the Academy
of Nutrition and Dietetics’ Pediatric Weight Management Evidence-Based Nutrition Practice Guidelines in their dietary or nutrition counselling of patients with type 2 DM at the time of diagnosis and as part of ongoing management.
6. Clinicians should encourage children and adolescents with type 2 DM to engage in moderate-to-vigorous exercise for at least 60 min daily and to limit nonacademic “screen time” to less than 2 h/d.
<25th percentile)