Page 1061 - TNFlipTest
P. 1061
Toronto Notes 2019
Endocrinology
Pediatrics P27
Epidemiology
• ~2.5%ofthepopulationbydefinition
Etiology
• seesidebar
Clinical Presentation
• historyandphysicalexam
■ plot on growth curve (special growth charts available for Turner syndrome, achondroplasia, DS)
■ assess for dysmorphic features, disproportionate short stature
■ risk factors for GH deficiency: previous head trauma, history of intracranial bleed or infection, head
surgery or irradiation, positive family history, breech delivery
■ decreased growth velocity may be more worrisome than actual height
• investigations
■ calculate mid-parental height: children are usually in a percentile between their parents’ height
(mid-parental height = (mother + father’s height in cm ± 12.5cm)/2)
■ AP x-ray of left hand and wrist for bone age
■ GHtesting
■ remaining investigations guided by history and physical (e.g. TSH, sweat chloride, etc.)
Management
• dependsonseverityofproblemasperceivedbyparents/child
• notreatmentfornon-pathologicalshortstature,exceptforidiopathicshortstature
• GHtherapyforGHdeficiency:ifadministeredatanearlyage,canhelppatientsachieveadultheight • requirements
■ GH shown to be deficient by 2 different stimulation tests (with argining, glucagon, insulin) ■ growth velocity <3rd percentile or height <<3rd percentile
■ bone age x-rays show unfused epiphyses/delayed bone age
• supportandmanagementofresultantself-imageissues,socialanxiety,etc.
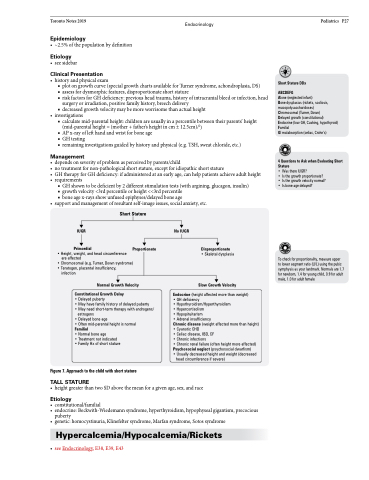
Short Stature DDx
ABCDEFG
Alone (neglected infant)
Bone dysplasias (rickets, scoliosis, mucopolysaccharidoses)
Chromosomal (Turner, Down)
Delayed growth (constitutional) Endocrine (low GH, Cushing, hypothyroid) Familial
GI malabsorption (celiac, Crohn’s)
4 Questions to Ask when Evaluating Short Stature
• Was there IUGR?
• Is the growth proportionate?
• Is the growth velocity normal? • Is bone age delayed?
To check for proportionality, measure upper to lower segment ratio (U/L) using the pubic symphysis as your landmark. Normals are 1.7 for newborn, 1.4 for young child, 0.9 for adult male, 1.0 for adult female
IUGR Primordial
• Height, weight, and head circumference are affected
No IUGR
Short Stature
Proportionate
Disproportionate
• Skeletal dysplasia
Slow Growth Velocity
• Chromosomal (e.g. Turner, Down syndrome) • Teratogen, placental insufficiency,
infection
Normal Growth Velocity
Constitutional Growth Delay
• Delayed puberty
• May have family history of delayed puberty
• May need short-term therapy with androgens/
estrogens
• Delayed bone age
• Often mid-parental height is normal Familial
• Normal bone age
• Treatment not indicated
• Family Hx of short stature
Figure 7. Approach to the child with short stature
TALL STATURE
Endocrine (height affected more than weight) • GH deficiency
• Hypothyroidism/Hyperthyroidism
• Hypercortisolism
• Hypopituitarism
• Adrenal insufficiency
Chronic disease (weight affected more than height) • Cyanotic CHD
• Celiac disease, IBD, CF
• Chronic infections
• Chronic renal failure (often height more affected) Psychosocial neglect (psychosocial dwarfism)
• Usually decreased height and weight (decreased
head circumference if severe)
• heightgreaterthantwoSDabovethemeanforagivenage,sex,andrace
Etiology
• constitutional/familial
• endocrine:Beckwith-Wiedemannsyndrome,hyperthyroidism,hypophysealgigantism,precocious
puberty
• genetic:homocystinuria,Klinefeltersyndrome,Marfansyndrome,Sotossyndrome
Hypercalcemia/Hypocalcemia/Rickets
• seeEndocrinology,E38,E39,E43