Page 1095 - TNFlipTest
P. 1095
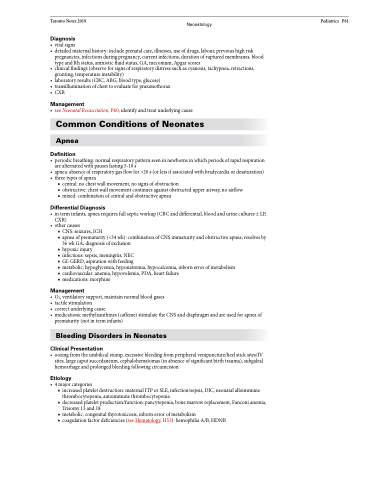
Toronto Notes 2019 Neonatology Pediatrics P61
Diagnosis
• vitalsigns
• detailedmaternalhistory:includeprenatalcare,illnesses,useofdrugs,labour,previoushighrisk
pregnancies, infections during pregnancy, current infections, duration of ruptured membranes, blood
type and Rh status, amniotic fluid status, GA, meconium, Apgar scores
• clinicalfindings(observeforsignsofrespiratorydistresssuchascyanosis,tachypnea,retractions,
grunting, temperature instability)
• laboratoryresults(CBC,ABG,bloodtype,glucose)
• transilluminationofchesttoevaluateforpneumothorax
• CXR
Management
• seeNeonatalResuscitation,P60,identifyandtreatunderlyingcause
Common Conditions of Neonates
Apnea
Definition
• periodicbreathing:normalrespiratorypatternseeninnewbornsinwhichperiodsofrapidrespiration are alternated with pauses lasting 5-10 s
• apnea:absenceofrespiratorygasflowfor>20s(orlessifassociatedwithbradycardiaordesaturation)
• threetypesofapnea
■ central: no chest wall movement, no signs of obstruction
■ obstructive: chest wall movement continues against obstructed upper airway, no airflow ■ mixed: combination of central and obstructive apnea
Differential Diagnosis
• interminfants,apnearequiresfullsepticworkup(CBCanddifferential,bloodandurinecultures±LP, CXR)
• othercauses
■ CNS: seizures, ICH
■ apnea of prematurity (<34 wk): combination of CNS immaturity and obstructive apnea; resolves by
36 wk GA; diagnosis of exclusion
■ hypoxic injury
■ infectious: sepsis, meningitis, NEC
■ GI: GERD, aspiration with feeding
■ metabolic: hypoglycemia, hyponatremia, hypocalcemia, inborn error of metabolism
■ cardiovascular: anemia, hypovolemia, PDA, heart failure
■ medications: morphine
Management
• O2,ventilatorysupport,maintainnormalbloodgases
• tactilestimulation
• correctunderlyingcause
• medications:methylxanthines(caffeine)stimulatetheCNSanddiaphragmandareusedforapneaof
prematurity (not in term infants)
Bleeding Disorders in Neonates
Clinical Presentation
• oozingfromtheumbilicalstump,excessivebleedingfromperipheralvenipuncture/heelsticksites/IV sites, large caput succedaneum, cephalohematomas (in absence of significant birth trauma), subgaleal hemorrhage and prolonged bleeding following circumcision
Etiology
• 4majorcategories
■ increased platelet destruction: maternal ITP or SLE, infection/sepsis, DIC, neonatal alloimmune
thrombocytopenia, autoimmune thrombocytopenia
■ decreased platelet production/function: pancytopenia, bone marrow replacement, Fanconi anemia,
Trisomy 13 and 18
■ metabolic: congenital thyrotoxicosis, inborn error of metabolism
■ coagulation factor deficiencies (see Hematology, H53): hemophilia A/B, HDNB