Page 1097 - TNFlipTest
P. 1097
Toronto Notes 2019 Neonatology Pediatrics P63
Treatment
• nogoodtreatments
• gradualweanfromventilator,optimizenutrition
• dexamethasonemayhelpdecreaseinflammationandencourageweaning,butuseofdexamethasoneis
associated with increased risk of adverse neurodevelopmental outcomes
Prognosis
• chronicrespiratoryfailuremayleadtopulmonaryHTN,poorgrowth,andright-sidedheartfailure
• patientswithbronchopulmonarydysplasiamaycontinuetohavesignificantimpairmentand
deterioration in lung function late into adolescence
• somelungabnormalitiesmaypersistintoadulthoodincludingairwayobstruction,airwayhyper-
reactivity, and emphysema
• associatedwithincreasedriskofadverseneurodevelopmentaloutcomes
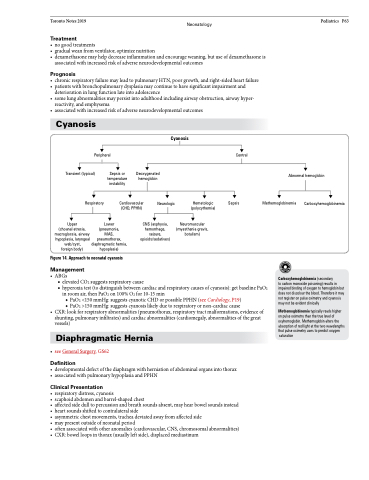
Cyanosis
Peripheral
Cyanosis
Transient (typical)
Respiratory
Sepsis or temperature instability
Deoxygenated hemoglobin
Central
Sepsis
Abnormal hemoglobin
Upper (choanal atresia, macroglossia, airway hypoplasia, laryngeal web/cyst, foreign body)
Lower (pneumonia, MAS, pneumothorax, diaphragmatic hernia, hypoplasia)
CNS (asphyxia, hemorrhage, seizure, opioids/sedatives)
Figure 14. Approach to neonatal cyanosis
Management
Cardiovascular Neurologic (CHD, PPHN)
Hematologic (polycythemia)
Neuromuscular (myasthenia gravis, botulism)
Methemoglobinemia
Carboxyhemoglobinemia
• ABGs
■ elevated CO2 suggests respiratory cause
■ hyperoxia test (to distinguish between cardiac and respiratory causes of cyanosis): get baseline PaO2
in room air, then PaO2 on 100% O2 for 10-15 min
◆ PaO2 <150 mmHg: suggests cyanotic CHD or possible PPHN (see Cardiology, P19) ◆ PaO2 >150 mmHg: suggests cyanosis likely due to respiratory or non-cardiac cause
• CXR:lookforrespiratoryabnormalities(pneumothorax,respiratorytractmalformations,evidenceof shunting, pulmonary infiltrates) and cardiac abnormalities (cardiomegaly, abnormalities of the great vessels)
Diaphragmatic Hernia
• seeGeneralSurgery,GS62
Definition
• developmentaldefectofthediaphragmwithherniationofabdominalorgansintothorax • associatedwithpulmonaryhypoplasiaandPPHN
Clinical Presentation
• respiratorydistress,cyanosis
• scaphoidabdomenandbarrel-shapedchest
• affectedsidedulltopercussionandbreathsoundsabsent,mayhearbowelsoundsinstead • heartsoundsshiftedtocontralateralside
• asymmetricchestmovements,tracheadeviatedawayfromaffectedside
• maypresentoutsideofneonatalperiod
• oftenassociatedwithotheranomalies(cardiovascular,CNS,chromosomalabnormalities) • CXR:bowelloopsinthorax(usuallyleftside),displacedmediastinum
Carboxyhemoglobinemia (secondary
to carbon monoxide poisoning) results in impaired binding of oxygen to hemoglobin but does not discolour the blood. Therefore it may not register on pulse oximetry and cyanosis may not be evident clinically
Methemoglobinemia typically reads higher on pulse oximetry than the true level of oxyhemoglobin. Methemoglobin alters the absorption of red light at the two wavelengths that pulse oximetry uses to predict oxygen
saturation