Page 1197 - TNFlipTest
P. 1197
Toronto Notes 2019
Personality Disorders
Psychiatry PS33
Epidemiology
• F:M=2:1
• beginsinadolescenceoryoung-adulthood
Treatment
• CBT
Avoidant/Restrictive Food Intake Disorder
Definition
• eating/feedingdisturbancetotheextentofpersistentfailuretomeetappropriatenutritionaland/or energy needs, resulting in significant weight loss/growth failure and nutritional deficiencies; patients experience disturbances in psychosocial functioning and may become dependent on enteral feeding/ oral nutritional supplementation
■ does not occur during an episode of AN or BN
■ no evidence of distress in the way in which one’s body weight or shape is experienced
Risk Factors
• temperament(e.g.anxietydisorders),environment(e.g.familialanxiety),genetic(e.g.historyofGI conditions)
Points for Differentiating Between Eating Disorders
• AN of binge-eating/purging type
(significantly low body weight) takes priority over a BN diagnosis (body weight not in criteria)
• BN requires compensatory behaviours • Binge eating disorder does not involve
compensatory behaviours
• Avoidant/restrictive food intake disorder
does not involve disturbances in body image
• beginsininfancyandcanpersistintoadulthood
Treatment
• psychoeducation
• behaviourmodification • psychotherapy
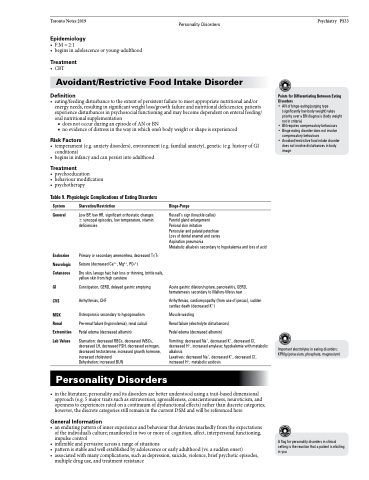
Table 9. Physiologic Complications of Eating Disorders
System
General
Endocrine Neurologic Cutaneous
GI
CVS
MSK
Renal Extremities Lab Values
Starvation/Restriction
Low BP, low HR, significant orthostatic changes ± syncopal episodes, low temperature, vitamin deficiencies
Primary or secondary amenorrhea, decreased T3/T4 Seizure (decreased Ca2+, Mg2+, PO43-)
Dry skin, lanugo hair, hair loss or thinning, brittle nails, yellow skin from high carotene
Constipation, GERD, delayed gastric emptying Arrhythmias, CHF
Osteoporosis secondary to hypogonadism Pre-renal failure (hypovolemia), renal calculi Pedal edema (decreased albumin)
Starvation: decreased RBCs, decreased WBCs, decreased LH, decreased FSH, decreased estrogen, decreased testosterone, increased growth hormone, increased cholesterol
Dehydration: increased BUN
Binge-Purge
Russell’s sign (knuckle callus) Parotid gland enlargement Perioral skin irritation
Periocular and palatal petechiae Loss of dental enamel and caries Aspiration pneumonia
Metabolic alkalosis secondary to hypokalemia and loss of acid
Acute gastric dilation/rupture, pancreatitis, GERD, hematemesis secondary to Mallory-Weiss tear
Arrhythmias, cardiomyopathy (from use of ipecac), sudden cardiac death (decreased K+)
Muscle wasting
Renal failure (electrolyte disturbances) Pedal edema (decreased albumin)
Vomiting: decreased Na+, decreased K+, decreased Cl-, decreased H+, increased amylase; hypokalemia with metabolic alkalosis
Laxatives: decreased Na+, decreased K+, decreased Cl-, increased H+; metabolic acidosis
Important electrolytes in eating disorders: KPMg (potassium, phosphate, magnesium)
Personality Disorders
• intheliterature,personalityanditsdisordersarebetterunderstoodusingatrait-baseddimensional approach (e.g. 5 major traits such as extraversion, agreeableness, conscientiousness, neuroticism, and openness to experiences rated on a continuum of dysfunctional effects) rather than discrete categories; however, the discrete categories still remain in the current DSM and will be referenced here
General Information
• anenduringpatternofinnerexperienceandbehaviourthatdeviatesmarkedlyfromtheexpectations of the individual’s culture; manifested in two or more of: cognition, affect, interpersonal functioning, impulse control
• inflexibleandpervasiveacrossarangeofsituations
• patternisstableandwellestablishedbyadolescenceorearlyadulthood(vs.asuddenonset)
• associatedwithmanycomplications,suchasdepression,suicide,violence,briefpsychoticepisodes,
A flag for personality disorders in clinical setting is the reaction that a patient is eliciting in you
multiple drug use, and treatment resistance