Page 124 - TNFlipTest
P. 124
CP2 Clinical Pharmacology
Acronyms
Toronto Notes 2019
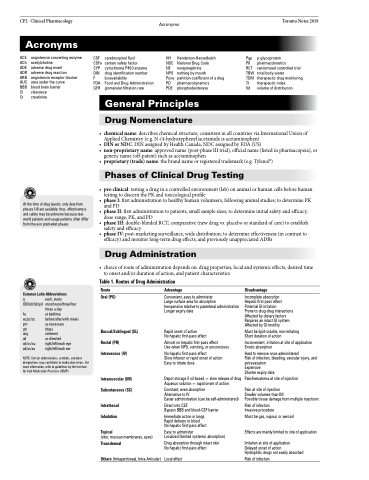
Acronyms
ACE angiotensin converting enzyme ACh acetylcholine
ADE adverse drug event
ADR adverse drug reaction
ARB angiotensin receptor blocker AUC area under the curve
BBB blood brain barrier
Cl clearance
Cr creatinine
CSF CSFa CYP DIN F FDA GFR
•
• •
•
• • • • •
•
cerebrospinal fluid
certain safety factor cytochrome P450 enzyme drug identification number bioavailability
Food and Drug Administration glomerular filtration rate
HH Henderson-Hasselbalch NDC National Drug Code
NE norepinephrine
NPO nothing by mouth
Po/w partition coefficient of a drug PD pharmacodynamics
PDE phosphodiesterase
Pgp p-glycoprotein
PK pharmacokinetics
RCT randomized controlled trial TBW total body water
TDM therapeutic drug monitoring TI therapeutic index
Vd volume of distribution
General Principles
Drug Nomenclature
At the time of drug launch, only data from phases I-III are available; thus, effectiveness and safety may be unknown because real- world patients and usage patterns often differ from those in premarket phases
Common Latin Abbreviations
q each, every OD/bid/tid/qid once/twice/three/four
times a day hs at bedtime
ac/pc/cc before/after/with meals prn as necessary
gtt drops
ung ointment
ud as directed od/os/ou right/left/each eye ad/as/au right/left/each ear
NOTE: Certain abbreviations, symbols, and dose designations may contribute to medication errors. For more information, refer to guidelines by the Institute for Safe Medication Practices (ISMP)
chemicalname:describeschemicalstructure;consistentinallcountriesviaInternationalUnionof Applied Chemistry (e.g. N-(4-hydroxyphenyl)acetamide is acetaminophen) DINorNDC:DINassignedbyHealthCanada;NDCassignedbyFDA(US) non-proprietaryname:approvedname(post-phaseIIItrial),officialname(listedinpharmacopeia),or generic name (off-patent) such as acetaminophen proprietary(trade)name:thebrandnameorregisteredtrademark(e.g.Tylenol®)
Phases of Clinical Drug Testing
pre-clinical:testingadruginacontrolledenvironment(lab)onanimalorhumancellsbeforehuman testing to discern the PK and toxicological profile phaseI:firstadministrationtohealthyhumanvolunteers,followinganimalstudies;todeterminePK and PD phaseII:firstadministrationtopatients,smallsamplesizes;todetermineinitialsafetyandefficacy, dose range, PK, and PD phaseIII:double-blindedRCT;comparative(newdrugvs.placeboorstandardofcare)toestablish safety and efficacy phaseIV:post-marketingsurveillance,widedistribution;todetermineeffectiveness(incontrastto efficacy) and monitor long-term drug effects, and previously unappreciated ADRs
Drug Administration
choiceofrouteofadministrationdependson:drugproperties,localandsystemiceffects,desiredtime to onset and/or duration of action, and patient characteristics
Table 1. Routes of Drug Administration
Route
Oral (PO)
Buccal/Sublingual (SL) Rectal (PR) Intravenous (IV)
Intramuscular (IM) Subcutaneous (SC)
Intrathecal Inhalation
Topical
(skin, mucous membranes, eyes)
Transdermal
Others (Intraperitoneal, Intra-Articular)
Advantage
Convenient, easy to administer
Large surface area for absorption
Inexpensive relative to parenteral administration Longer expiry date
Rapid onset of action
No hepatic first-pass effect
Almost no hepatic first-pass effect
Use when NPO, vomiting, or unconscious
No hepatic first-pass effect
Slow infusion or rapid onset of action Easy to titrate dose
Depot storage if oil-based = slow release of drug Aqueous solution = rapid onset of action
Constant, even absorption
Alternative to IV
Easier administration (can be self-administered)
Direct into CSF
Bypass BBB and blood-CSF barrier
Immediate action in lungs Rapid delivery to blood
No hepatic first-pass effect
Easy to administer
Localized (limited systemic absorption)
Drug absorption through intact skin No hepatic first-pass effect
Local effect
Disadvantage
Incomplete absorption
Hepatic first-pass effect Potential GI irritation
Prone to drug-drug interactions Affected by dietary factors Requires an intact GI system Affected by GI motility
Must be lipid-soluble, non-irritating Short duration of action
Inconvenient, irritation at site of application Erratic absorption
Hard to remove once administered
Risk of infection, bleeding, vascular injury, and extravasation
Expensive
Shorter expiry date
Pain/hematoma at site of injection
Pain at site of injection
Smaller volumes than IM
Possible tissue damage from multiple injections
Risk of infection Invasive procedure
Must be gas, vapour, or aerosol
Effects are mainly limited to site of application
Irritation at site of application Delayed onset of action
Hydrophilic drugs not easily absorbed
Risk of infection