Page 1258 - TNFlipTest
P. 1258
R12 Respirology
Airway Disease Toronto Notes 2019 Bronchiectasis
Definition
• irreversibledilatationofairwaysduetoinflammatorydestructionofairwaywallsresultingfrom persistently infected mucus
• usuallyaffectsmediumsizedairways
• themostcommonsputumpathogensinnon-cysticfibrosispatientsareH.influenzae,P.aeruginosa,and
M. catarrhalis
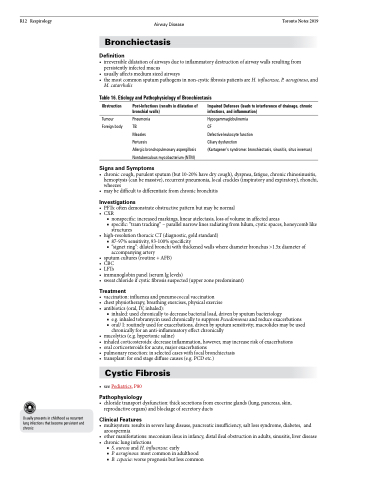
Table 16. Etiology and Pathophysiology of Bronchiectasis
Obstruction
Tumour Foreign body
Post-Infectious (results in dilatation of bronchial walls)
Pneumonia
TB
Measles
Pertussis
Allergic bronchopulmonary aspergillosis Nontuberculous mycobacterium (NTM)
Impaired Defenses (leads to interference of drainage, chronic infections, and inflammation)
Hypogammaglobulinemia
CF
Defective leukocyte function
Ciliary dysfunction
(Kartagener’s syndrome: bronchiectasis, sinusitis, situs inversus)
Usually presents in childhood as recurrent lung infections that become persistent and chronic
• chroniccough,purulentsputum(but10-20%havedrycough),dyspnea,fatigue,chronicrhinosinusitis, hemoptysis (can be massive), recurrent pneumonia, local crackles (inspiratory and expiratory), rhonchi, wheezes
• maybedifficulttodifferentiatefromchronicbronchitis
Investigations
• PFTs:oftendemonstrateobstructivepatternbutmaybenormal • CXR
■ nonspecific: increased markings, linear atelectasis, loss of volume in affected areas
■ specific: “tram tracking” – parallel narrow lines radiating from hilum, cystic spaces, honeycomb like
structures
• high-resolutionthoracicCT(diagnostic,goldstandard)
■ 87-97%sensitivity,93-100%specificity
■ “signet ring”: dilated bronchi with thickened walls where diameter bronchus >1.5x diameter of
accompanying artery
• sputumcultures(routine+AFB)
• CBC
• LFTs
• immunoglobinpanel(serumIglevels)
• sweatchlorideifcysticfibrosissuspected(upperzonepredominant)
Treatment
• vaccination:influenzaandpneumococcalvaccination
• chestphysiotherapy,breathingexercises,physicalexercise • antibiotics(oral,IV,inhaled):
■ inhaled: used chronically to decrease bacterial load, driven by sputum bacteriology
■ e.g. inhaled tobramycin used chronically to suppress Pseudomonas and reduce exacerbations
■ oral/ I: routinely used for exacerbations, driven by sputum sensitivity; macrolides may be used
chronically for an anti-inflammatory effect chronically
• mucolytics(e.g.hypertonicsaline)
• inhaledcorticosteroids:decreaseinflammation,however,mayincreaseriskofexacerbations • oralcorticosteroidsforacute,majorexacerbations
• pulmonaryresection:inselectedcaseswithfocalbronchiectasis
• transplant:forendstagediffusecauses(e.g.PCDetc.)
Cystic Fibrosis
• seePediatrics,P80
Pathophysiology
• chloridetransportdysfunction:thicksecretionsfromexocrineglands(lung,pancreas,skin, reproductive organs) and blockage of secretory ducts
Clinical Features
• multisystem: results in severe lung disease, pancreatic insufficiency, salt loss syndrome, diabetes, and azoospermia
• othermanifestations:meconiumileusininfancy,distalilealobstructioninadults,sinusitis,liverdisease
• chroniclunginfections
■ S. aureus and H. influenzae: early
■ P. aeruginosa: most common in adulthood
■ B. cepacia: worse prognosis but less common
Signs and Symptoms