Page 1257 - TNFlipTest
P. 1257
Toronto Notes 2019
Airway Disease
Respirology R11
Surgery
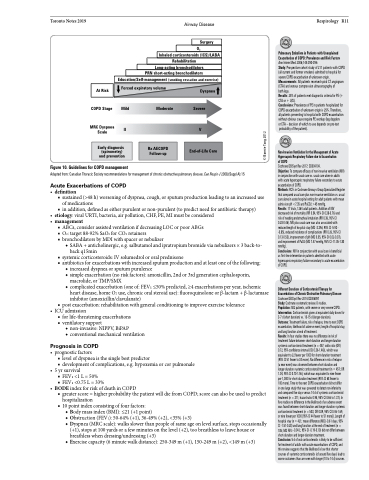
O2
Inhaled corticosteroids (ICS)/LABA
Rehabilitation
Long-acting bronchodilators
PRN short-acting bronchodilators
Education/Self-management (smoking cessation and exercise)
At Risk
Forced expiratory volume
Dyspnea
Pulmonary Embolism in Patients with Unexplained Exacerbation of COPD: Prevalence and Risk Factors Ann Intern Med 2006;144:390-396
Study: Prospective cohort study of 211 patients with COPD (all current and former smokers) admitted to hospital for severe COPD exacerbation of unknown origin. Measurements: All patients received spiral CT angiogram (CTA) and venous compression ultrasonography of
both legs.
Results: 25% of patients met diagnostic criteria for PE (+ CTA or + U/S).
Conclusions: Prevalence of PE in patients hospitalized for COPD exacerbation of unknown origin is 25%. Therefore, all patients presenting to hospital with COPD exacerbation without obvious cause require PE workup (leg dopplers or CTA – decision of which to use depends on pre-test probability of the patient).
Non-Invasive Ventilation for the Management of Acute Hypercapnic Respiratory Failure due to Exacerbation of COPD
Cochrane DB Syst Rev 2017; CD004104.
Objective: To compare efficacy of non-invasive ventilation (NIV) in conjunction with usual care vs. usual care alone in adults with acute hypercapnic respiratory failure secondary to acute exacerbation of COPD.
Methods: RCTs in Cochrane Airways Group Specialized Register that compared usual care plus non-invasive ventilation vs. usual care alone in acute hospital setting for adult patients with mean admission pH <7.35 and PaCO2 >45 mmHg.
Results: 17 trials, 1264 adult patients. Addition of NIV decreased risk of mortality (RR 0.54, 95% CI 0.38-0.76) and risk of needing endotracheal intubation (RR 0.36, 95% CI 0.28-0.46). NIV plus usual care was also associated with reduced length of hospital stay (MD -3.39d, 95% CI -5.93 - -0.85), reduced incidence of complications (RR 0.26, 95% CI 0.13-0.53), improvement of pH (MD 0.05, 95% CI 0.02-0.07), and improvement of PaO2 (MD 7.47 mmHg, 95% CI -11.05-1.80 mmHg).
Conclusions: NIV in conjunction with usual care is beneficial as first-line intervention in patients admitted with acute hypercapnic respiratory failure secondary to acute exacerbation of COPD.
Different Durations of Corticosteroid Therapy for Exacerbations of Chronic Obstructive Pulmonary Disease Cochrane DB Syst Rev 2014:CD006897
Study: Cochrane systematic review. 8 studies.
Population: 582 patients, with severe or very severe COPD. Intervention: Corticosteroids given at equivalent daily doses for 3-7 d (short duration) vs. 10-15 d (longer-duration).
Outcome: Treatment failure, risk of relapse, time to next COPD exacerbation, likelihood of adverse event, length of hospital stay, and lung function at end of treatment.
Results: In four studies there was no difference in risk of treatment failure between short-duration and longer-duration systemic corticosteroid treatment (n =457; odds ratio (OR) 0.72, 95% confidence interval (CI) 0.36-1.46)), which was equivalent to 22 fewer per 1000 for short-duration treatment (95% CI 51 fewer to 34 more). No difference in risk of relapse (a new event) was observed between short-duration and longer-duration systemic corticosteroid treatment (n =457; OR 1.04, 95% CI 0.70-1.56), which was equivalent to nine fewer per 1,000 for short-duration treatment (95% CI 68 fewer to
100 more). Time to the next COPD exacerbation did not differ
in one large study that was powered to detect non-inferiority and compared five days versus 14 d of systemic corticosteroid treatment (n = 311; hazard ratio 0.95, 95% CI 0.66 to 1.37). In five studies no difference in the likelihood of an adverse event was found between short-duration and longer-duration systemic corticosteroid treatment (n = 503; OR 0.89, 95% CI 0.46-1.69, or nine fewer per 1000 [95% CI 44 fewer to 51 more]). Length of hospital stay (n =421; mean difference (MD) -0.61 days, 95% CI -1.51-0.28) and lung function at the end of treatment (n = 185;MDFEV1 -0.04L;95%CI-0.19-0.10)didnotdifferbetween short-duration and longer-duration treatment.
Conclusion: 5 d of oral corticosteroids is likely to be sufficient for treatment of adults with acute exacerbations of COPD, and this review suggests that the likelihood is low that shorter courses of systemic corticosteroids (of around five days) lead to worse outcomes than are seen with longer (10 to 14 d) courses.
COPD Stage
MRC Dyspnea Scale
II V
Mild Moderate Severe
Early diagnosis (spirometry) and prevention
Rx AECOPD Follow-up
Figure 10. Guidelines for COPD management
Adapted from: Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease. Can Respir J 2008;(Suppl A):15
Acute Exacerbations of COPD
• definition
■ sustained (>48 h) worsening of dyspnea, cough, or sputum production leading to an increased use
of medications
■ in addition, defined as either purulent or non-purulent (to predict need for antibiotic therapy)
• etiology:viralURTI,bacteria,airpollution,CHF,PE,MImustbeconsidered • management
■ ABCs, consider assisted ventilation if decreasing LOC or poor ABGs ■ O2: target 88-92% SaO2 for CO2 retainers
■ bronchodilators by MDI with spacer or nebulizer
◆ SABA + anticholinergic, e.g. salbutamol and ipratropium bromide via nebulizers × 3 back-to- back q15min
■ systemic corticosteroids: IV solumedrol or oral prednisone
■ antibiotics for exacerbations with increased sputum production and at least one of the following:
◆ increased dyspnea or sputum purulence
◆ simple exacerbation (no risk factors): amoxicillin, 2nd or 3rd generation cephalosporin,
macrolide, or TMP/SMX
◆ complicated exacerbation (one of: FEV1 ≤50% predicted, ≥4 exacerbations per year, ischemic
heart disease, home O2 use, chronic oral steroid use): fluoroquinolone or β-lactam + β-lactamase
inhibitor (amoxicillin/clavulanate)
■ post exacerbation: rehabilitation with general conditioning to improve exercise tolerance
• ICUadmission
■ for life-threatening exacerbations ■ ventilatory support
◆ non-invasive: NIPPV, BiPAP
◆ conventional mechanical ventilation
Prognosis in COPD
• prognosticfactors
■ level of dyspnea is the single best predictor
■ development of complications, e.g. hypoxemia or cor pulmonale
• 5yrsurvival
■ FEV1<1L=50%
■ FEV1<0.75L=33%
• BODEindexforriskofdeathinCOPD
■ greater score = higher probability the patient will die from COPD; score can also be used to predict
hospitalization
■ 10 point index consisting of four factors:
◆ Body mass index (BMI): ≤21 (+1 point)
◆ Obstruction (FEV1): 50-64% (+1), 36-49% (+2), <35% (+3)
◆ Dyspnea (MRC scale): walks slower than people of same age on level surface, stops occasionally
(+1), stops at 100 yards or a few minutes on the level (+2), too breathless to leave house or
breathless when dressing/undressing (+3)
◆ Exercise capacity (6 minute walk distance): 250-349 m (+1), 150-249 m (+2), <149 m (+3)
End-of-Life Care
© Bonnie Tang 2012