Page 1255 - TNFlipTest
P. 1255
Toronto Notes 2019
Airway Disease
Respirology R9
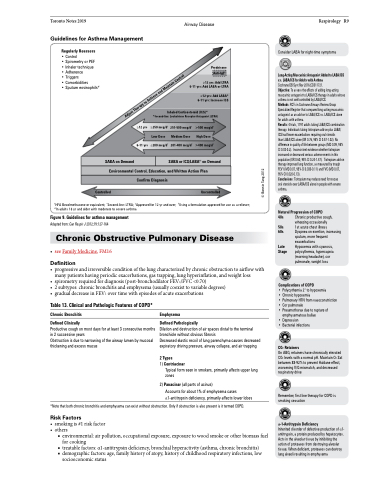
Guidelines for Asthma Management
Regularly Reassess
• Control
• Spirometry or PEF
• Inhaler technique
• Adherence
• Triggers
• Comorbidities
• Sputum eosinophils#
Prednisone Anti-IgE‡
≥12 yrs: Add LTRA 6-11 yrs: Add LABA or LTRA
≥12 yrs: Add LABA* 6-11 yrs: Increase ICS
Inhaled Corticosteroid (ICS)* *Second-line: Leukotriene Receptor Antagonist (LTRA)
Consider LABA for night-time symptoms
Long-Acting Muscarinic Antagonist Added to LABA/ICS v.s. LABA/ICS for Adults with Asthma
Cochrane DB Syst Rev 2016;CD011721.
Objective: To assess the effects of adding long-acting muscarinic antagonist to LABA/ICS therapy in adults whose asthma is not well controlled by LABA/ICS.
Methods: RCTs in Cochrane Airways Review Group Specialized Register that compared long-acting muscarinic antagonist as an add-on to LABA/ICS vs. LABA/ICS alone for adults with asthma.
Results: 4 trials, 1197 adults taking LABA/ICS combination therapy. Individuals taking tiotropium add-on plus LABA/ ICS had fewer exacerbations requiring oral steroids
than LABA/ICS alone (OR 0.76, 95% CI 0.57-1.02). No difference in quality of life between groups (MD 0.09, 95% CI0.03-0.2). Inconsistentevidencewhethertiotropium increased or decreased serious adverse events in this population(OR0.60,95%CI0.24-1.47). Tiotropiumadd-on therapy improved lung function, as measured by trough FEV1 (MD 0.07, 95% CI 0.030-0.11) and FVC (MD 0.07, 95% CI 0.020-0.13).
Conclusions: Tiotropium may reduce need for rescue
oral steroids over LABA/ICS alone in people with severe asthma.
Natural Progression of COPD
40s Chronic productive cough,
wheezing occasionally 50s 1st acute chest illness
60s Dyspnea on exertion, increasing sputum, more frequent
exacerbations
Late Hypoxemia with cyanosis, Stage polycythemia, hypercapnia
(morning headache), cor pulmonale, weight loss
Complications of COPD
• Polycythemia 2° to hypoxemia
• Chronic hypoxemia
• Pulmonary HTN from vasoconstriction
• Cor pulmonale
• Pneumothorax due to rupture of
emphysematous bullae
• Depression
• Bacterial infections
CO2 Retainers
On ABG, retainers have chronically elevated CO2 levels with a normal pH. Maintain O2 Sat between 88-92% to prevent Haldane effect, worsening V/Q mismatch, and decreased respiratory drive
Remember, first line therapy for COPD is smoking cessation
α-1-Antitrypsin Deficiency
Inherited disorder of defective production of α1- antitrypsin, a protein produced by hepatocytes. Acts in the alveolar tissue by inhibiting the action of proteases from destroying alveolar tissue. When deficient, proteases can destroy lung alveoli resulting in emphysema
≥12 yrs
6-11 yrs
≥250 mcg/d† Low Dose ≤200 mcg/d†
251-500 mcg/d† Medium Dose 201-400 mcg/d†
>500 mcg/d† High Dose >400 mcg/d†
Uncontrolled
SABA on Demand
SABAorICS/LABAঠonDemand
Environmental Control, Education, and Written Action Plan
Confirm Diagnosis
Controlled
†HFA Becolmethasone or equivalent; *Second-line: LTRA; ‡Approved for 12 yr and over; ¶Using a formulation approved for use as a reliever; #In adults 18 yr and older with moderate to severe asthma
Figure 9. Guidelines for asthma management
Adapted from: Can Respir J 2012;19:127-164
Chronic Obstructive Pulmonary Disease
• seeFamilyMedicine,FM16
Definition
• progressiveandirreversibleconditionofthelungcharacterizedbychronicobstructiontoairflowwith many patients having periodic exacerbations, gas trapping, lung hyperinflation, and weight loss
• spirometryrequiredfordiagnosis(post-bronchodilatorFEV1/FVC<0.70)
• 2subtypes:chronicbronchitisandemphysema(usuallycoexisttovariabledegrees)
• gradual decrease in FEV1 over time with episodes of acute exacerbations
Table 13. Clinical and Pathologic Features of COPD*
Chronic Bronchitis Defined Clinically
Productive cough on most days for at least 3 consecutive months in 2 successive years
Obstruction is due to narrowing of the airway lumen by mucosal thickening and excess mucus
Emphysema
Defined Pathologically
Dilation and destruction of air spaces distal to the terminal bronchiole without obvious fibrosis
Decreased elastic recoil of lung parenchyma causes decreased expiratory driving pressure, airway collapse, and air trapping
2 Types
1) Centriacinar
Typical form seen in smokers, primarily affects upper lung zones
2) Panacinar (all parts of acinus)
Accounts for about 1% of emphysema cases α1-antitrypsin deficiency, primarily affects lower lobes
*Note that both chronic bronchitis and emphysema can exist without obstruction. Only if obstruction is also present is it termed COPD.
Risk Factors
• smokingis#1riskfactor • others
■ environmental: air pollution, occupational exposure, exposure to wood smoke or other biomass fuel for cooking
■ treatable factors: α1-antitrypsin deficiency, bronchial hyperactivity (asthma, chronic bronchitis) ■ demographic factors: age, family history of atopy, history of childhood respiratory infections, low
socioeconomic status
Adjust Therapy to Achieve and Maintain Control
© Bonnie Tang 2012