Page 1253 - TNFlipTest
P. 1253
Toronto Notes 2019
Airway Disease
Respirology R7
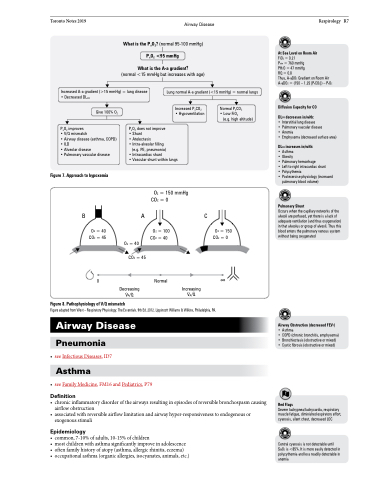
What is the PaO2? (normal 95-100 mmHg) PaO2 <95 mmHg
What is the A-a gradient?
(normal <15 mmHg but increases with age)
At Sea Level on Room Air
FiO2 = 0.21
Patm = 760 mmHg
PH2O = 47 mmHg
RQ=0.8
Thus, A-aDO2 Gradient on Room Air A-aDO2 = (150 – 1.25 [PaCO2]) – PaO2
Diffusion Capacity for CO
DLCO decreases in/with:
• Interstitial lung disease
• Pulmonary vascular disease
• Anemia
• Emphysema (decreased surface area)
DLCO increases in/with:
• Asthma
• Obesity
• Pulmonary hemorrhage
• Left-to-right intracardiac shunt
• Polycythemia
• Postexercise physiology (increased
pulmonary blood volume)
Pulmonary Shunt
Occurs when the capillary networks of the alveoli are perfused, yet there is a lack of adequate ventilation (and thus oxygenation) in that alveolus or group of alveoli. Thus this blood enters the pulmonary venous system without being oxygenated
Increased A-a gradient (>15 mmHg) = lung disease • Decreased DLCO
Lung normal A-a gradient (<15 mmHg) = normal lungs
Give 100% O2
PaO2 improves
• V/Q mismatch
• Airway disease (asthma, COPD) • ILD
• Alveolar disease
• Pulmonary vascular disease
Figure 7. Approach to hypoxemia
Increased PaCO2 • Hypoventilation
Normal PaCO2 • Low FiO2
(e.g. high altitude)
PaO2 does not improve • Shunt
• Atelectasis
• Intra-alveolar filling
(e.g. PE, pneumonia)
• Intracardiac shunt
• Vascular shunt within lungs
O2 = 150 mmHg CO2 = 0
B
A
CO2 = 45
Decreasing
C
Figure 8. Pathophysiology of V/Q mismatch
O2 = 40 CO2 = 45
0
O2 = 40
O2 = 100 CO2 = 40
Normal
O2 = 150 CO2 = 0
∞
.. ..
VA/Q VA/Q
Figure adapted from West – Respiratory Physiology: The Essentials. 9th Ed. 2012. Lippincott Williams & Wilkins, Philadelphia, PA.
Airway Disease
Pneumonia
• seeInfectiousDiseases,ID7
Asthma
• seeFamilyMedicine,FM16andPediatrics,P79
Definition
Airway Obstruction (decreased FEV1)
• Asthma
• COPD (chronic bronchitis, emphysema) • Bronchiectasis (obstructive or mixed) • Cystic fibrosis (obstructive or mixed)
Red Flags
Severe tachypnea/tachycardia, respiratory muscle fatigue, diminished expiratory effort, cyanosis, silent chest, decreased LOC
Central cyanosis is not detectable until SaO2 is <85%. It is more easily detected in polycythemia and less readily detectable in anemia
Increasing
• chronicinflammatorydisorderoftheairwaysresultinginepisodesofreversiblebronchospasmcausing airflow obstruction
• associatedwithreversibleairflowlimitationandairwayhyper-responsivenesstoendogenousor exogenous stimuli
Epidemiology
• common,7-10%ofadults,10-15%ofchildren
• mostchildrenwithasthmasignificantlyimproveinadolescence
• oftenfamilyhistoryofatopy(asthma,allergicrhinitis,eczema)
• occupationalasthma(organicallergies,isocyanates,animals,etc.)