Page 1251 - TNFlipTest
P. 1251
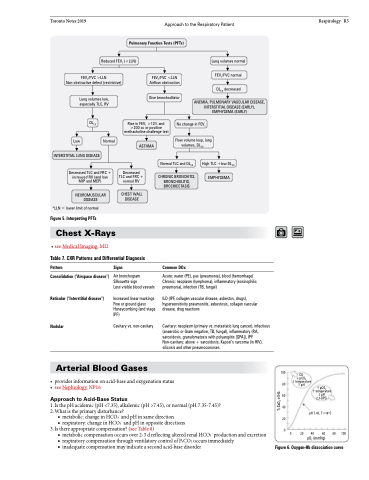
Toronto Notes 2019 Approach to the Respiratory Patient Pulmonary Function Tests (PFTs)
Respirology R5
Reduced FEV1 (<LLN)
Lung volumes normal
FEV1/FVC normal
DLCO decreased
ANEMIA, PULMONARY VASCULAR DISEASE, INTERSTITIAL DISEASE (EARLY), EMPHYSEMA (EARLY)
FEV1/FVC >LLN Non-obstructive defect (restrictive)
Lung volumes low, especially TLC, RV
FEV1/FVC <LLN Airflow obstruction
Give bronchodilator
DLCO
Low
Normal
Rise in FEV1 >12% and >200 cc or positive methacholine challenge test
ASTHMA
Decreased TLC and FRC + normal RV
CHEST WALL DISEASE
No change in FEV1
Flow volume loop, lung volumes, DLCO
INTERSTITIAL LUNG DISEASE
Decreased TLC and FRC + increased RV (and low MIP and MEP)
NEUROMUSCULAR DISEASE
*LLN = lower limit of normal
Figure 5. Interpreting PFTs
Chest X-Rays
Normal TLC and DLCO
CHRONIC BRONCHITIS, BRONCHIOLITIS, BROCHIECTASIS
High TLC +low DLCO
EMPHYSEMA
• see Medical Imaging, MI2
Table 7. CXR Patterns and Differential Diagnosis
Pattern
Consolidation (“Airspace disease”)
Reticular (“Interstitial disease”)
Nodular
Signs
Air bronchogram Silhouette sign
Less visible blood vessels
Increased linear markings Fine or ground glass Honeycombing (end stage IPF)
Cavitary vs. non-cavitary
Common DDx
• providesinformationonacid-baseandoxygenationstatus • see Nephrology, NP16
Approach to Acid-Base Status
1. Is the pH acidemic (pH <7.35), alkalemic (pH >7.45), or normal (pH 7.35-7.45)? 2. What is the primary disturbance?
■ metabolic: change in HCO3- and pH in same direction
i pCO 2
Acute: water (PE), pus (pneumonia), blood (hemorrhage) Chronic: neoplasm (lymphoma), inflammatory (eosinophilic pneumonia), infection (TB, fungal)
ILD (IPF, collagen vascular disease, asbestos, drugs), hypersensitivity pneumonitis, asbestosis, collagen vascular disease, drug reactions
Cavitary: neoplasm (primary vs. metastatic lung cancer), infectious (anaerobic or Gram negative, TB, fungal), inflammatory (RA, sarcoidosis, granulomatosis with polyangiitis [GPA]), IPF Non-cavitary: above + sarcoidosis, Kaposi’s sarcoma (in HIV), silicosis and other pneumoconioses
Arterial Blood Gases
100
i temperature 80 h pH
CO
■ respiratory: change in HCO3- and pH in opposite directions
3. Is there appropriate compensation? (see Table 8) 0
pH 7.40, T=38oC
0 20 40 60 80 100 pO2 (mmHg)
■ metabolic compensation occurs over 2-3 d reflecting altered renal HCO3- production and excretion ■ respiratory compensation through ventilatory control of PaCO2 occurs immediately
■ inadequatecompensationmayindicateasecondacid-basedisorder
Figure6.Oxygen-Hbdissociationcurve
60 40 20
h pCO2
h temperature ipH 2,3-DPG
% SaO2 of Hb