Page 1325 - TNFlipTest
P. 1325
Toronto Notes 2019
Lower Urinary Tract Symptoms (LUTS)
Urology U7
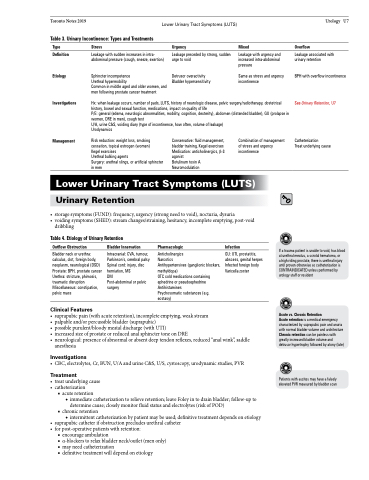
Table 3. Urinary Incontinence: Types and Treatments
Type
Definition
Etiology
Investigations
Management
Stress
Leakage with sudden increases in intra- abdominal pressure (cough, sneeze, exertion)
Sphincter incompetence
Urethral hypermobility
Common in middle aged and older women, and men following prostate cancer treatment
Urgency
Leakage preceded by strong, sudden urge to void
Detrusor overactivity Bladder hypersensitivity
Mixed
Leakage with urgency and increased intra-abdominal pressure
Same as stress and urgency incontinence
Overflow
Leakage associated with urinary retention
BPH with overflow incontinence
See Urinary Retention, U7
Catheterization
Treat underlying cause
Hx: when leakage occurs, number of pads, LUTS, history of neurologic disease, pelvic surgery/radiotherapy, obstetrical history, bowel and sexual function, medications, impact on quality of life
P/E: general (edema, neurologic abnormalities, mobility, cognition, dexterity), abdomen (distended bladder), GU (prolapse in women, DRE in men), cough test
U/A, urine C&S, voiding diary (type of incontinence, how often, volume of leakage) Urodynamics
Risk reduction: weight loss, smoking cessation, topical estrogen (women) Kegel exercises
Urethral bulking agents
Surgery: urethral slings, or artificial sphincter in men
Conservative: fluid management, bladder training, Kegel exercises Medication: anticholinergics, β-3 agonist
Botulinum toxin A Neuromodulation
Combination of management of stress and urgency incontinence
Lower Urinary Tract Symptoms (LUTS)
Urinary Retention
• storagesymptoms(FUND):frequency,urgency(strongneedtovoid),nocturia,dysuria
• voidingsymptoms(SHED):streamchanges/straining,hesitancy,incompleteemptying,post-void
dribbling
Table 4. Etiology of Urinary Retention
Outflow Obstruction
Bladder neck or urethra: calculus, clot, foreign body, neoplasm, neurological (DSD) Prostate: BPH, prostate cancer Urethra: stricture, phimosis, traumatic disruption Miscellaneous: constipation, pelvic mass
Clinical Features
Bladder Innervation
Intracranial: CVA, tumour, Parkinson’s, cerebral palsy Spinal cord: injury, disc herniation, MS
DM
Post-abdominal or pelvic surgery
Pharmacologic
Anticholinergics
Narcotics
Antihypertensives (ganglionic blockers, methyldopa)
OTC cold medications containing ephedrine or pseudoephedrine Antihistamines
Psychosomatic substances (e.g. ecstasy)
Infection
GU: UTI, prostatitis, abscess, genital herpes Infected foreign body Varicella zoster
If a trauma patient is unable to void, has blood at urethral meatus, a scrotal hematoma, or
a high riding prostate, there is urethral injury until proven otherwise so catheterization is CONTRAINDICATED unless performed by urology staff or resident
Acute vs. Chronic Retention
Acute retention is a medical emergency characterized by suprapubic pain and anuria with normal bladder volume and architecture Chronic retention can be painless with greatly increased bladder volume and detrusor hypertrophy followed by atony (late)
Patients with ascites may have a falsely elevated PVR measured by bladder scan
• suprapubicpain(withacuteretention),incompleteemptying,weakstream • palpableand/orpercussiblebladder(suprapubic)
• possiblepurulent/bloodymeataldischarge(withUTI)
• increased size of prostate or reduced anal sphincter tone on DRE
• neurological: presence of abnormal or absent deep tendon reflexes, reduced “anal wink”, saddle anesthesia
Investigations
• CBC,electrolytes,Cr,BUN,U/AandurineC&S,U/S,cystoscopy,urodynamicstudies,PVR
Treatment
• treatunderlyingcause • catheterization
■ acute retention
◆ immediate catheterization to relieve retention; leave Foley in to drain bladder; follow-up to
determine cause; closely monitor fluid status and electrolytes (risk of POD) ■ chronic retention
◆ intermittent catheterization by patient may be used; definitive treatment depends on etiology • suprapubiccatheterifobstructionprecludesurethralcatheter
• forpost-operativepatientswithretention:
■ encourage ambulation
■ α-blockers to relax bladder neck/outlet (men only) ■ may need catheterization
■ definitive treatment will depend on etiology