Page 1335 - TNFlipTest
P. 1335
Toronto Notes 2019 Infectious and Inflammatory Diseases Epididymitis and Orchitis
Etiology
• commoninfectiouscauses
■ <35 yr: N. gonorrhoeae or Chlamydia trachomatis
■ ≥35 yr or penetrative anal intercourse: GI organisms (especially E. coli)
• othercauses
■ mumps infection may involve orchitis, post-parotitis ■ TB
■ syphilis
■ granulomatous (autoimmune) in elderly men
■ amiodarone (involves only head of epididymis)
■ chemical: reflux of urine into ejaculatory ducts
Risk Factors
• UTI
• unprotectedsexualcontact
• instrumentation/catheterization
• increasedpressureinprostaticurethra(straining,voiding,heavylifting)maycauserefluxofurinealong
vas deferens → sterile epididymitis • immunocompromise
Clinical Features
• suddenonsetscrotalpainandswelling±radiationalongcordtoflank • scrotalerythemaandtenderness
• Prehn’sSign(reliefofpainwithliftingoftesticle)
• fever
• storagesymptoms,purulentd/c • reactivehydrocele
Investigations
• U/A,urineC&S
• ±urethrald/c:Gramstain/culture
• ifdiagnosisuncertain,MUSTruleouttesticulartorsion(U/SDoppler)
Treatment
• ruleouttorsion(seeInvestigationsTable23,U31) • seeTable8,U13forABxtherapy
• scrotalsupport,bedrest,ice,analgesia
Complications
• ifsevere→testicularatrophy
• 30%havepersistentinfertilityproblems
• inadequatelytreatedacuteepididymitismayleadtochronicepididymitisorepididymo-orchitis
Urology U17
If unsure between diagnoses of epididymitis and torsion, always go to OR
Remember: torsion >6 h has poor prognosis
Urethritis
Etiology
• infectiousorinflammatory(e.g.reactivearthritis)
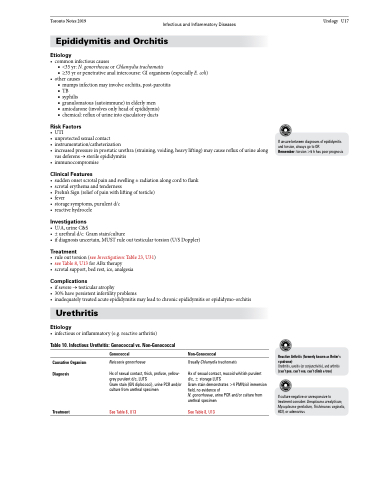
Table 10. Infectious Urethritis: Gonococcal vs. Non-Gonococcal
Causative Organism Diagnosis
Treatment
Gonococcal
Neisseria gonorrhoeae
Hx of sexual contact, thick, profuse, yellow- grey purulent d/c, LUTS
Gram stain (GN diplococci), urine PCR and/or culture from urethral specimen
See Table 8, U13
Non-Gonococcal
Usually Chlamydia trachomatis
Hx of sexual contact, mucoid whitish purulent
d/c, ± storage LUTS
Gram stain demonstrates >4 PMN/oil immersion field, no evidence of
N. gonorrhoeae, urine PCR and/or culture from urethral specimen
See Table 8, U13
Reactive Arthritis (formerly known as Reiter’s syndrome)
Urethritis, uveitis (or conjunctivitis), and arthritis (can’t pee, can’t see, can’t climb a tree)
If culture negative or unresponsive to treatment consider: Ureaplasma urealyticum, Mycoplasma genitalium, Trichimonas vaginalis, HSV, or adenovirus