Page 1346 - TNFlipTest
P. 1346
U28 Urology
Urological Neoplasms
Toronto Notes 2019
Long-Term Follow-Up on PSA Screening
Lancet 2014:384(9959):2027-2035
Summary: With 13 yr follow-up, the mortality reduction remains unchanged (21%, and 29% after non-compliance adjustment). However, the number needed to screen and to treat is decreasing, and is now below the number needed to screen observed in breast cancer trials.
Methods: multi-centre RCT with predefined central database, analysis, and core age group (55-69 years) evaluating PSA in 8 European countries. Incidence and mortality truncated at 9, 11, and
13 years follow-up in the intervention arm was compared to control arm.
Results: RR of PCa incidence between intervention and control arms was 1.91 after 9 yr follow-up, 1.66 at 11 year follow-up, and 1.67 at 13 yr follow- up. RR of PCa mortality was 0.85, 0.78, and 0.79, at 9, 11, 13 yr follow-up, respectively. RRR is 21%, and ARR from death is 1.28 per 1000 men.
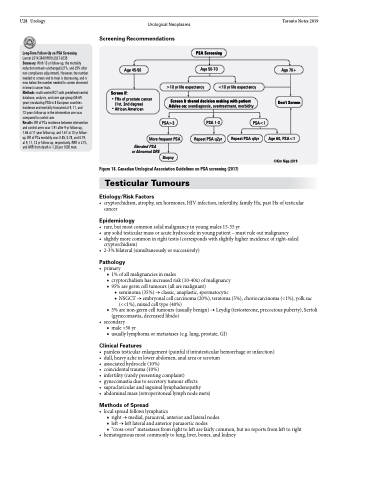
Screening Recommendations
Age 45-50
Screen if:
FHx of prostate cancer (1st, 2nd degree) African American
PSA Screening
Age 50-70
>10 yr life expectancy
<10 yr life expectancy
Age 70+
Don’t Screen
Age 60, PSA<1
©Kim Nipp 2019
Screen & shared decision making with patient Advise on: overdiagnosis, overtreatment, morbidity
PSA>3
PSA 1-3
Repeat PSA q2yr
PSA<1
Repeat PSA q4yr
More frequent PSA
Elevated PSA or Abnormal DRE
Biopsy
Figure 18. Canadian Urological Association Guidelines on PSA screening (2017)
Testicular Tumours
Etiology/Risk Factors
• cryptorchidism,atrophy,sexhormones,HIVinfection,infertility,familyHx,pastHxoftesticular cancer
Epidemiology
• rare,butmostcommonsolidmalignancyinyoungmales15-35yr
• anysolidtesticularmassoracutehydrocoeleinyoungpatient–mustruleoutmalignancy
• slightlymorecommoninrighttestis(correspondswithslightlyhigherincidenceofright-sided
cryptorchidism)
• 2-3%bilateral(simultaneouslyorsuccessively)
Pathology
• primary
■ 1% of all malignancies in males
■ cryptorchidism has increased risk (10-40x) of malignancy ■ 95% are germ cell tumours (all are malignant)
◆ seminoma (35%) → classic, anaplastic, spermatocytic
◆ NSGCT → embryonal cell carcinoma (20%), teratoma (5%), choriocarcinoma (<1%), yolk sac
(<<1%), mixed cell type (40%)
■ 5% are non-germ cell tumours (usually benign) → Leydig (testosterone, precocious puberty), Sertoli
(gynecomastia, decreased libido) • secondary
■ male >50 yr
■ usually lymphoma or metastases (e.g. lung, prostate, GI)
Clinical Features
• painlesstesticularenlargement(painfulifintratesticularhemorrhageorinfarction) • dull,heavyacheinlowerabdomen,analareaorscrotum
• associatedhydrocele(10%)
• coincidentaltrauma(10%)
• infertility(rarelypresentingcomplaint)
• gynecomastiaduetosecretorytumoureffects
• supraclavicularandinguinallymphadenopathy
• abdominalmass(retroperitoneallymphnodemets)
Methods of Spread
• localspreadfollowslymphatics
■ right → medial, paracaval, anterior and lateral nodes
■ left → left lateral and anterior paraaortic nodes
■ “cross-over” metastases from right to left are fairly common, but no reports from left to right
• hematogenousmostcommonlytolung,liver,bones,andkidney