Page 1345 - TNFlipTest
P. 1345
Toronto Notes 2019
Urological Neoplasms
Urology U27
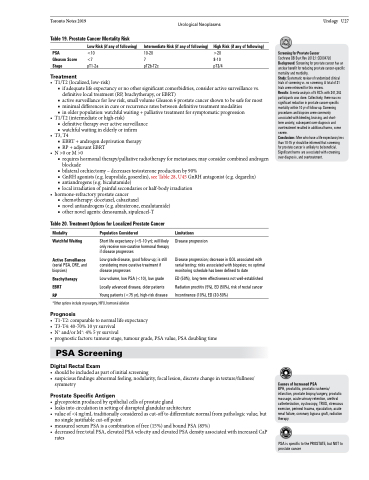
Table 19. Prostate Cancer Mortality Risk
PSA
Gleason Score Stage
Treatment
Low Risk (if any of following)
<10 <7 pT1-2a
Intermediate Risk (if any of following)
10-20
7 pT2b-T2c
High Risk (if any of following)
>20 8-10 pT3/4
Screening for Prostate Cancer
Cochrane DB Syst Rev 2013;1:CD004720 Background: Screening for prostate cancer has an unclear benefit for reducing prostate cancer-specific mortality and morbidity.
Study: Systematic review of randomized clinical trials of screening vs. no screening. A total of 31 trials were retrieved for this review.
Results: A meta-analysis of 5 RCTs with 341,342 participants was done. Collectively, there was no significant reduction in prostate cancer-specific mortality within 10 yr of follow-up. Screening procedures and biopsies were commonly associated with bleeding, bruising, and short-
term anxiety; subsequent over-diagnosis and overtreatment resulted in additional harms, some severe.
Conclusions: Men who have a life expectancy less than 10-15 yr should be informed that screening
for prostate cancer is unlikely to be beneficial. Significant harms are associated with screening, over-diagnosis, and overtreatment.
• T1/T2(localized,low-risk)
■ if adequate life expectancy or no other significant comorbidities, consider active surveillance vs.
definitive local treatment (RP, brachytherapy, or EBRT)
■ active surveillance for low risk, small volume Gleason 6 prostate cancer shown to be safe for most
■ minimal differences in cure or recurrence rates between definitive treatment modalities ■ in older population: watchful waiting + palliative treatment for symptomatic progression
• T1/T2(intermediateorhigh-risk)
■ definitive therapy over active surveillance ■ watchful waiting in elderly or infirm
• T3,T4
■ EBRT+androgendeprivationtherapy ■ RP + adjuvant EBRT
• N>0orM>0
■ requires hormonal therapy/palliative radiotherapy for metastases; may consider combined androgen
blockade
■ bilateral orchiectomy – decreases testosterone production by 90%
■ GnRH agonists (e.g. leuprolide, goserelin), see Table 28, U45 GnRH antagonist (e.g. degarelix)
■ antiandrogens (e.g. bicalutamide)
■ local irradiation of painful secondaries or half-body irradiation
• hormone-refractoryprostatecancer
■ chemotherapy: docetaxel, cabazitaxel
■ novel antiandrogens (e.g. abiraterone, enzalutamide) ■ other novel agents: denosumab, sipuleucel-T
Table 20. Treatment Options for Localized Prostate Cancer
Modality
Watchful Waiting Active Surveillance
(serial PSA, DRE, and biopsies)
Brachytherapy EBRT
RP
Population Considered
Short life expectancy (<5-10 yr); will likely only receive non-curative hormonal therapy if disease progresses
Low grade disease, good follow-up; is still considering more curative treatment if disease progresses
Low volume, low PSA (<10), low grade Locally advanced disease, older patients Young patients (<75 yr), high-risk disease
Limitations
Disease progression
Disease progression; decrease in QOL associated with serial testing; risks associated with biopsies; no optimal monitoring schedule has been defined to date
ED (50%), long-term effectiveness not well-established Radiation proctitis (5%), ED (50%), risk of rectal cancer Incontinence (10%), ED (30-50%)
*Other options include cryosurgery, HIFU, hormonal ablation
Prognosis
• T1-T2:comparabletonormallifeexpectancy
• T3-T4:40-70%10yrsurvival
• N+ and/or M+: 4% 5 yr survival
• prognosticfactors:tumourstage,tumourgrade,PSAvalue,PSAdoublingtime
PSA Screening
Digital Rectal Exam
• shouldbeincludedaspartofinitialscreening
• suspiciousfindings:abnormalfeeling,nodularity,focallesion,discretechangeintexture/fullness/
symmetry
Prostate Specific Antigen
• glycoproteinproducedbyepithelialcellsofprostategland
• leaks into circulation in setting of disrupted glandular architecture
• value of <4 ng/mL traditionally considered as cut-off to differentiate normal from pathologic value, but
no single justifiable cut-off point
• measuredserumPSAisacombinationoffree(15%)andboundPSA(85%)
• decreasedfree:totalPSA,elevatedPSAvelocityandelevatedPSAdensityassociatedwithincreasedCaP
rates
Causes of Increased PSA
BPH, prostatitis, prostatic ischemia/ infarction, prostate biopsy/surgery, prostatic massage, acute urinary retention, urethral catheterization, cystoscopy, TRUS, strenuous exercise, perineal trauma, ejaculation, acute renal failure, coronary bypass graft, radiation therapy
PSA is specific to the PROSTATE, but NOT to prostate cancer