Page 1343 - TNFlipTest
P. 1343
Toronto Notes 2019 Urological Neoplasms Staging
• forinvasivedisease:CTorMRI,CXR,LFTs,extendedelectrolytes(Ca2+,Mg2+,PO43–)(metastaticworkup)
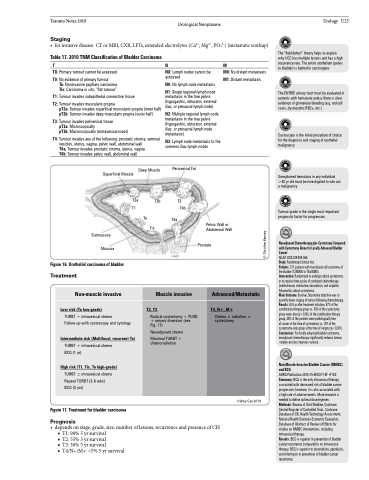
Table 17. 2010 TNM Classification of Bladder Carcinoma
TNM
Urology U25
The “field defect” theory helps to explain why UCC has multiple lesions and has a high recurrence rate. The entire urothelium (pelvis to bladder) is bathed in carcinogens
The ENTIRE urinary tract must be evaluated in patients with hematuria unless there is clear evidence of glomerular bleeding (e.g. red cell casts, dysmorphic RBCs, etc.)
Cystoscopy is the initial procedure of choice for the diagnosis and staging of urothelial malignancy
Unexplained hematuria in any individual >40 yr old must be investigated to rule out a malignancy
Tumour grade is the single most important prognostic factor for progression
Neoadjuvant Chemotherapy plus Cystectomy Compared with Cystectomy Alone for Locally Advanced Bladder Cancer
NEJM2003;349:859-866
Study: Randomized clinical trial.
Patients: 317 patients with transitional-cell carcinoma of the bladder (T2N0M0 to T4aN0M0).
Intervention: Randomized to undergo radical cystectomy or to receive three cycles of combined chemotherapy (methotrexate, vinblastine, doxorubicin, and cisplatin) followed by radical cystectomy.
Main Outcome: Survival. Secondary objective was to quantify down-staging of tumour following chemotherapy. Results: At 5 yr after treatment initiation, 57% of the combination-therapy group vs. 43% of the cystectomy group were alive (p=0.06). In the combination-therapy group, 38% of the patients were pathologically free
of cancer at the time of cystectomy vs. 15% of the cystectomy-only group at the time of surgery (p<0.001). Conclusions: For locally advanced bladder carcinoma, neoadjuvant chemotherapy significantly reduces tumour volume and also improves survival.
Non-Muscle-Invasive Bladder Cancer (NMIBC) and BCG
AHRQ Publication 2015:15-EHC017-EF #153 Summary: BCG is the only intravesical therapy associated with decreased risk of bladder cancer progression; however, it is also associated with
a high rate of adverse events. More research is needed to define optimal dose/regimen. Methods: Review of Ovid Medline, Cochrane Central Register of Controlled Trials, Cochrane Database of SR, Health Technology Assessment, National Health Sciences Economic Evaluation, Database of Abstract of Review of Effects for studies on NMIBC interventions, including intravesicaltherapy. Results:BCGissuperiorinpreventionofbladder cancer recurrence compared to no intravesical therapy. BCG is superior to doxorubicin, epirubicin, and mitomycin in prevention of bladder cancer recurrence.
TX: Primary tumour cannot be assessed
T0: No evidence of primary tumour
Ta: Noninvasive papillary carcinoma Tis: Carcinoma in situ: “flat tumour”
T1: Tumour invades subepithelial connective tissue
T2: Tumour invades muscularis propria
pT2a: Tumour invades superficial muscularis propria (inner half) pT2b: Tumour invades deep muscularis propria (outer half)
T3: Tumour invades perivesical tissue
pT3a: Microscopically
pT3b: Macroscopically (extravesical mass)
T4: Tumour invades any of the following: prostatic stroma, seminal vesicles, uterus, vagina, pelvic wall, abdominal wall
T4a: Tumour invades prostatic stroma, uterus, vagina
T4b: Tumour invades pelvic wall, abdominal wall
Deep Muscle Superficial Muscle
NX: Lymph nodes cannot be assessed
N0: No lymph node metastasis N1: Single regional lymph node
metastasis in the true pelvis (hypogastric, obturator, external iliac, or presacral lymph node)
N2: Multiple regional lymph node metastasis in the true pelvis (hypogastric, obturator, external iliac, or presacral lymph node metastasis)
N3: Lymph node metastasis to the common iliac lymph nodes
M0: No distant metastasis M1: Distant metastasis
T2a T1
T2b
Ta
Tis
Perivesical Fat
T3 T4b
T4a
Pelvic Wall or Abdominal Wall
Submucosa Mucosa
Figure 16. Urothelial carcinoma of bladder
Prostate
Treatment
Treatment of Bladder Carcinoma
Non-muscle invasive
Muscle invasive
Advanced/Metastatic
Low risk (Ta low-grade)
TURBT + intravesical chemo
Follow-up with cystoscopy and cytology
Intermediate risk (Multifocal, recurrent Ta)
TURBT + intravesical chemo BCG (1 yr)
High risk (T1, Tis, Ta high-grade)
TURBT ± intravesical chemo Repeat TURBT (2-6 wks) BCG (3 yrs)
T2, T3
Radical cystectomy + PLND + urinary diversion (see
Fig. 17)
Neoadjuvant chemo
Maximal TURBT + chemoradiation
T4, N+, M+
Chemo ± radiation ± cystectomy
Figure 17. Treatment for bladder carcinoma
Prognosis
• dependsonstage,grade,size,numberoflesions,recurrenceandpresenceofCIS ■ T1:90%5yrsurvival
■ T2:55%5yrsurvival
■ T3: 30% 5 yr survival
■ T4/N+/M+: <5% 5 yr survival
©Amy Cao 2019
© Christine Kenney