Page 214 - TNFlipTest
P. 214
ER34 Emergency Medicine
Medical Emergencies Toronto Notes 2019
• admitifhemodynamicallyunstable,requiresupplementalO2,majorcomorbidities,lackofsufficient social supports, unable to ambulate, need invasive therapy
■ referral to medicine for coagulopathy and malignancy workup
50% of patients with symptomatic proximal DVT will develop PE, often within days to weeks of the event
Oral Rivaroxaban for the Treatment of Symptomatic Pulmonary Embolism
NEJM 2012;366:1287-97
Purpose: To evaluate the use of rivaroxaban alone as anticoagulation therapy for acute PE.
Methods: A randomized, open-label, event-driven, non-inferiority trial was undertaken to compare rivaroxaban (15 mg twice daily for 3 wk, followed by 20 mg once daily) with standard therapy of enoxaparin followed by an adjusted-dose vitamin K antagonist, in patients with acute symptomatic PE with or without DVT.
Results: 4,832 patients were enrolled. Rivaroxaban was non-inferior to standard therapy (non-inferiority margin, 2.0; p=0.003) for preventing recurrent
VTE (HR: 1.12; 95% CI 0.75-1.68). Major bleeding occurred less in the rivaroxaban group (hazard ratio, 0.49; 0.31-0.79; p=0.003). Rates of other adverse events were similar in the two groups. Conclusions: A fixed-dose regimen of rivaroxaban alone was non-inferior to standard therapy for the initial and long-term treatment of PE.
Oral Rivaroxaban for the Treatment of Symptomatic Venous Thromboembolism
NEJM2010;363:2499-2510
Purpose: To compare the efficacy and safety of rivaroxaban with standard therapy (enoxaparin, Vitamin K antagonist) or placebp in patients with acute symptomatic DVT, and in patients with confirmed symptomatic DVT or PE previously treated with a Vitamin K antagonist or rivaroxaban for
6 to 12 mo.
Methods: Acute DVT Study was a randomized, open-label trial comparing rivaroxaban to standard therapy consisting of enoxaparin and a vitamin K antagonist in patients with acute, symptomatic DVT. The Continued Treatment Study (EINSTEIN–Extension) was a double-blind study in which patients with confirmed symptomatic DVT or pulmonary embolism who had been treated for 6 or 12 mo with
a vitamin K antagonist or rivaroxaban were randomly assigned to receive continued treatment with rivaroxaban or placebo. Primary efficacy outcome for both studies
was symptomatic, recurrent VTE (composite of DVT, non-fatal and fatal PE). For the Acute DVT Study, primary safety outcome was clinically relevant bleeding; for the EINSETIN-Extension study, the primary safety outcome was major bleeding.
Results: 3,449 (1,731 rivaroxaban, 1,718 enoxaparin/ Vitamin K antagonist) and 1,197 (602 rivaroxaban, 594 placebo) patients participated in the two trials, respectively. Rivaroxaban had non-inferior efficacy with respect to recurrent VTE (HR: 0.68 95%CI: 0.44-1.04). Similar bleeding prevalence were reported in each group. In the parallel continued-treatment study, rivaroxaban had superior efficacy with respect to preventing VTE (HR: 0.18 95%CI 0.09-0.39). Four patients in the rivaroxaban group had nonfatal major bleeding vs. none in the placebo group (p=0.11).
Conclusions: Rivaroxaban offers a single-drug approach
to treatment of VTE that may improve the benefit-to-risk profile of anticoagulation.
Normal
Repeat U/S in 5 days
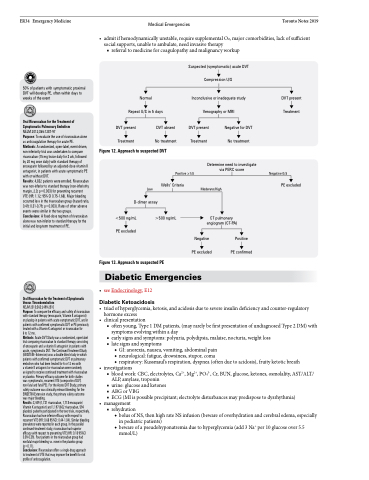
Suspected (symptomatic) acute DVT Compression U/S
Inconclusive or inadequate study
Venography or MRI
DVT present
Treatment
Negative 0/8
PE excluded
DVT present Treatment
DVT absent No treatment
DVT present Treatment
Negative for DVT No treatment
Figure 12. Approach to suspected DVT
Positive ≥1/8 Wells’ Criteria
Low
D-dimer assay
Determine need to investigate via PERC score
Moderate/High
CT pulmonary angiogram (CT-PA)
<500 ng/mL PE excluded
>500 ng/mL
Negative PE excluded
Positive PE confirmed
Figure 13. Approach to suspected PE
Diabetic Emergencies
• seeEndocrinology,E12 Diabetic Ketoacidosis
• triadofhyperglycemia,ketosis,andacidosisduetosevereinsulindeficiencyandcounter-regulatory
•
•
•
hormone excess clinical presentation
■ often young, Type 1 DM patients, (may rarely be first presentation of undiagnosed Type 2 DM) with symptoms evolving within a day
■ early signs and symptoms: polyuria, polydipsia, malaise, nocturia, weight loss ■ late signs and symptoms
◆ GI: anorexia, nausea, vomiting, abdominal pain
◆ neurological: fatigue, drowsiness, stupor, coma
◆ respiratory: Kussmaul’s respiration, dyspnea (often due to acidosis), fruity ketotic breath
investigations
■ blood work: CBC, electrolytes, Ca2+, Mg2+, PO43-, Cr, BUN, glucose, ketones, osmolality, AST/ALT/
ALP, amylase, troponin
■ urine: glucose and ketones
■ ABGorVBG
■ ECG (MI is possible precipitant; electrolyte disturbances may predispose to dysrhythmia)
management
■ rehydration
◆ bolus of NS, then high rate NS infusion (beware of overhydration and cerebral edema, especially in pediatric patients)
◆ beware of a pseudohyponatremia due to hyperglycemia (add 3 Na+ per 10 glucose over 5.5 mmol/L)