Page 249 - TNFlipTest
P. 249
Toronto Notes 2019 Disorders of Glucose Metabolism Diabetes Mellitus
Definition
• diabetesmellitusisaheterogeneousmetabolicdisordercharacterizedbythepresenceof hyperglycemia due to impairment of insulin secretion, defective insulin action, or both
• chronichyperglycemiaofdiabetesisassociatedwithrelativelyspecificlong-termmicrovascular complications affecting the eyes, kidneys and nerves, as well as an increased risk for cardiovascular disease
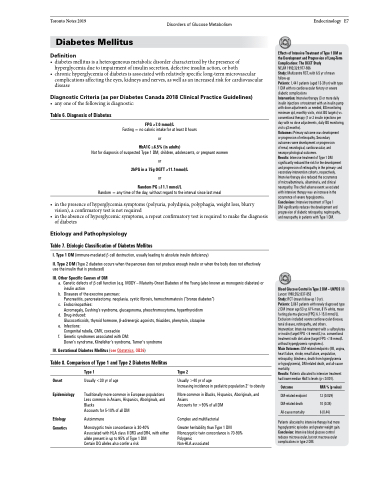
Diagnostic Criteria (as per Diabetes Canada 2018 Clinical Practice Guidelines)
• anyoneofthefollowingisdiagnostic:
Endocrinology E7
Effects of Intensive Treatment of Type 1 DM on the Development and Progression of Long-Term Complications: The DCCT Study
NEJM 1993;329:977-986
Study: Multicentre RCT, with 6.5 yr of mean follow-up
Patients: 1,441 patients (aged 13-39 yr) with type 1 DM with no cardiovascular history or severe diabetic complications
Intervention: Intensive therapy (3 or more daily insulin injections or treatment with an insulin pump with dose adjustments as needed, BG monitoring minimum qid, monthly visits, strict BG targets) vs. conventional therapy (1 or 2 insulin injections per day with no dose adjustments, daily BG monitoring, visits q3 months).
Outcomes: Primary outcome was development or progression of retinopathy. Secondary outcomes were development or progression
of renal, neurological, cardiovascular, and neuropsychological outcomes.
Results: Intensive treatment of Type 1 DM significantly reduced the risk for the development and progression of retinopathy in the primary- and secondary-intervention cohorts, respectively. Intensive therapy also reduced the occurrence
of microalbuminuria, albuminuria, and clinical neuropathy. The chief adverse event associated with intensive therapy was an increase in the occurrence of severe hypoglycemia. Conclusions: Intensive treatment of Type 1
DM significantly reduces the development and progression of diabetic retinopathy, nephropathy, and neuropathy in patients with Type 1 DM.
Blood Glucose Control in Type 2 DM – UKPDS 33
Lancet 1998;352:837-853
Study: RCT (mean follow-up 10 yr).
Patients: 3,867 patients with newly diagnosed type 2 DM (mean age 53 yr, 61% men, 81% white, mean fasting plasma glucose [FPG] 6.1-15.0 mmol/L). Exclusions included severe cardiovascular disease, renal disease, retinopathy, and others.
Intervention: Intensive treatment with a sulfonylurea or insulin (target FPG <6 mmol/L) vs. conventional treatment with diet alone (target FPG <15 mmol/L without hyperglycemic symptoms).
Main Outcomes: DM-related endpoints (MI, angina, heart failure, stroke, renal failure, amputation, retinopathy, blindness, death from hyperglycemia
or hypoglycemia), DM-related death, and all-cause mortality.
Results: Patients allocated to intensive treatment had lower median HbA1c levels (p<0.001).
Table 6. Diagnosis of Diabetes
FPG ≥7.0 mmol/L
Fasting = no caloric intake for at least 8 hours
or
HbA1C ≥6.5% (in adults)
Not for diagnosis of suspected Type 1 DM, children, adolescents, or pregnant women
or
2hPG in a 75g OGTT ≥11.1mmol/L or
Random PG ≥11.1 mmol/L
Random = any time of the day, without regard to the interval since last meal
• inthepresenceofhyperglycemiasymptoms(polyuria,polydipsia,polyphagia,weightloss,blurry vision), a confirmatory test is not required
• in the absence of hyperglycemic symptoms, a repeat confirmatory test is required to make the diagnosis of diabetes
Etiology and Pathophysiology
Table 7. Etiologic Classification of Diabetes Mellitus
I. Type 1 DM (immune-mediated β cell destruction, usually leading to absolute insulin deficiency)
II. Type 2 DM (Type 2 diabetes occurs when the pancreas does not produce enough insulin or when the body does not effectively use the insulin that is produced)
III. Other Specific Causes of DM
a. Genetic defects of β cell function (e.g. MODY – Maturity-Onset Diabetes of the Young (also known as monogenic diabetes) or insulin action
b. Diseases of the exocrine pancreas:
Pancreatitis, pancreatectomy, neoplasia, cystic fibrosis, hemochromatosis (“bronze diabetes”)
c. Endocrinopathies:
Acromegaly, Cushing’s syndrome, glucagonoma, pheochromocytoma, hyperthyroidism
d. Drug-induced:
Glucocorticoids, thyroid hormone, β-adrenergic agonists, thiazides, phenytoin, clozapine
e. Infections:
Congenital rubella, CMV, coxsackie
f. Genetic syndromes associated with DM:
Down’s syndrome, Klinefelter’s syndrome, Turner’s syndrome
IV. Gestational Diabetes Mellitus (see Obstetrics, OB26)
Table 8. Comparison of Type 1 and Type 2 Diabetes Mellitus
Type 1
Usually <30 yr of age
Traditionally more common in European populations Less common in Asians, Hispanics, Aboriginals, and Blacks
Accounts for 5-10% of all DM
Autoimmune
Monozygotic twin concordance is 30-40%
Associated with HLA class II DR3 and DR4, with either allele present in up to 95% of Type 1 DM
Certain DQ alleles also confer a risk
Type 2
Usually >40 yr of age
Increasing incidence in pediatric population 2o to obesity
More common in Blacks, Hispanics, Aboriginals, and Asians
Accounts for >90% of all DM
Complex and multifactorial
Greater heritability than Type 1 DM Monozygotic twin concordance is 70-90% Polygenic
Non-HLA associated
Onset Epidemiology
Etiology Genetics
Outcome
DM-related endpoint DM-related death All-cause mortality
RRR % (p value)
12 (0.029) 10 (0.34) 6 (0.44)
Patients allocated to intensive therapy had more hypoglycemic episodes and greater weight gain. Conclusion: Intensive blood glucose control reduces microvascular, but not macrovascular complications in type 2 DM.