Page 257 - TNFlipTest
P. 257
Toronto Notes 2019 Obesity
Cataracts
• subcapsularandsenilecataractssecondarytoglycosylatedlensproteinorincreasedsorbitolcausing osmotic change and fibrosis
Infections
• seeInfectiousDiseases,ID15
Hypoglycemia (BG <4.0 mmol/L or 72 mg/dL)
Etiology and Pathophysiology
• hypoglycemiaoccursmostfrequentlyinpeoplewithDMreceivinginsulinorcertainantihyperglycemic therapies (insulin secretagogues)
• inpeoplewithoutDM,caremustbetakentodistinguishfastingfrompost-prandialhypoglycemiaas each invokes separate differential diagnoses
Endocrinology E15
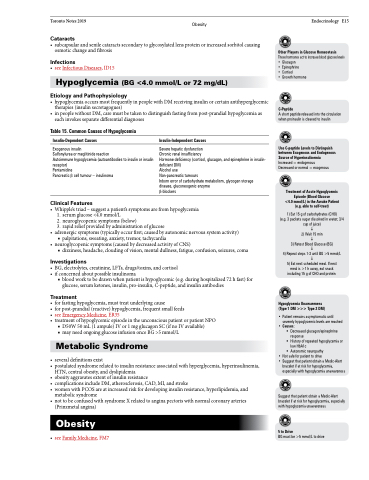
Table 15. Common Causes of Hypoglycemia
Insulin-Dependent Causes
Exogenous insulin
Sulfonylurea or meglitinide reaction
Autoimmune hypoglycemia (autoantibodies to insulin or insulin receptor)
Pentamidine
Pancreatic β cell tumour – insulinoma
Clinical Features
Insulin-Independent Causes
Severe hepatic dysfunction
Chronic renal insufficiency
Hormone deficiency (cortisol, glucagon, and epinephrine in insulin- deficient DM)
Alcohol use
Non-pancreatic tumours
Inborn error of carbohydrate metabolism, glycogen storage disease, gluconeogenic enzyme
β-blockers
Other Players in Glucose Homeostasis
These hormones act to increase blood glucose levels • Glucagon
• Epinephrine
• Cortisol
• Growth hormone
C-Peptide
A short peptide released into the circulation when proinsulin is cleaved to insulin
Use C-peptide Levels to Distinguish between Exogenous and Endogenous Source of Hyperinsulinemia Increased = endogenous
Decreased or normal = exogenous
Treatment of Acute Hypoglycemic Episode (Blood Glucose <4.0 mmol/L) in the Awake Patient (e.g. able to self-treat)
1) Eat 15 g of carbohydrates (CHO) (e.g. 3 packets sugar dissolved in water; 3/4 cup of juice)
2) Wait 15 min
3) Retest Blood Glucose (BG)
4) Repeat steps 1-3 until BG >5 mmol/L
5) Eat next scheduled meal. If next meal is >1 h away, eat snack including 15 g of CHO and protein
Hypoglycemia Unawareness (Type 1 DM >>> Type 2 DM)
• Patient remains asymptomatic until severely hypoglycemic levels are reached
• Causes:
Decreased glucagon/epinephrine
response
History of repeated hypoglycemia or
low HbA1c
Autonomic neuropathy
• Not safe for patient to drive
• Suggest that patient obtain a Medic-Alert
bracelet if at risk for hypoglycemia, especially with hypoglycemia unawareness
Suggest that patient obtain a Medic-Alert bracelet if at risk for hypoglycermia, especially with hypoglycemia unawareness
5 to Drive
BG must be >5 mmol/L to drive
• Whipple’striad–suggestapatient’ssymptomsarefromhypoglycemia 1. serum glucose <4.0 mmol/L
2. neuroglycopenic symptoms (below)
3. rapid relief provided by administration of glucose
• adrenergicsymptoms(typicallyoccurfirst;causedbyautonomicnervoussystemactivity) ■ palpitations, sweating, anxiety, tremor, tachycardia
• neuroglycopenicsymptoms(causedbydecreasedactivityofCNS)
■ dizziness, headache, clouding of vision, mental dullness, fatigue, confusion, seizures, coma
Investigations
• BG,electrolytes,creatinine,LFTs,drugs/toxins,andcortisol • ifconcernedaboutpossibleinsulinoma
■ blood work to be drawn when patient is hypoglycemic (e.g. during hospitalized 72 h fast) for glucose, serum ketones, insulin, pro-insulin, C-peptide, and insulin antibodies
Treatment
• forfastinghypoglycemia,musttreatunderlyingcause
• for post-prandial (reactive) hypoglycemia, frequent small feeds
• seeEmergencyMedicine,ER35
• treatment of hypoglycemic episode in the unconscious patient or patient NPO
■ D50W 50 mL (1 ampule) IV or 1 mg glucagon SC (if no IV available) ■ may need ongoing glucose infusion once BG >5 mmol/L
Metabolic Syndrome
• severaldefinitionsexist
• postulated syndrome related to insulin resistance associated with hyperglycemia, hyperinsulinemia,
HTN, central obesity, and dyslipidemia
• obesityaggravatesextentofinsulinresistance
• complicationsincludeDM,atherosclerosis,CAD,MI,andstroke
• womenwithPCOSareatincreasedriskfordevelopinginsulinresistance,hyperlipidemia,and
metabolic syndrome
• not to be confused with syndrome X related to angina pectoris with normal coronary arteries
(Prinzmetal angina)
Obesity
• seeFamilyMedicine,FM7