Page 278 - TNFlipTest
P. 278
E36 Endocrinology Disorders of Multiple Endocrine Glands Toronto Notes 2019
MEN I – Wermer’s Syndrome Affects the3Ps
Pituitary Parathyroid Pancreas
• othersigns:orthostatichypotension,papilledema,hyperglycemia,dilatedcardiomyopathy
• symptomsmaybetriggeredbystress,exertion,anesthesia,abdominalpressure,certainfoods(especially
tyramine containing foods – such as aged/strong cheese and cured meats)
Investigations
• urinecatecholamines
■ increased catecholamine metabolites (metanephrines) and free catecholamines ■ plasma metanephrines if available (most sensitive)
◆ cut-off values will depend on assay used • CTabdomen
■ ifnegative,wholebodyCTandmeta-iodo-benzoguanidine(MIBG)scintigraphy,Octreoscan,orMRI
Treatment
• surgicalremovaloftumour(curative)withcarefulpre-andpost-operativeICUmonitoring • adequatepre-operativepreparation
■ α-blockade for BP control: doxazosin or calcium channel blockers (10-21 d pre-operative), IV phentolamine (perioperative, if required)
■ β-blockade for HR control once α blocked for a few days
■ metyrosine (catecholamine synthesis inhibitor) + phenoxybenzamine or prazosin ■ volume restoration with vigorous salt-loading and fluids
• rescreenurine1-3mopost-operatively
• screenurineinfirstdegreerelatives;genetictestinginpatients<50yr
Disorders of Multiple Endocrine Glands
Multiple Endocrine Neoplasm
• neoplasticsyndromesinvolvingmultipleendocrineglands
• tumoursofneuroectodermalorigin
• autosomaldominantinheritancewithvariablepenetrance
• geneticscreeningforRETproto-oncogeneonchromosome10haslong-termbenefitinMENII
■ early cure and prevention of medullary thyroid cancer
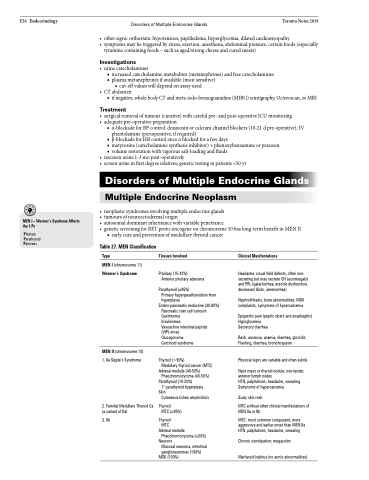
Table 27. MEN Classification
Type
MEN I (chromosome 11) Wermer’s Syndrome
Tissues Involved
Pituitary (15-42%)
Anterior pituitary adenoma
Parathyroid (≥95%)
Primary hyperparathyroidism from hyperplasia
Entero-pancreatic endocrine (30-80%) Pancreatic islet cell tumours Gastrinoma
Insulinomas
Vasoactive intestinal peptide (VIP)-omas
Glucagonoma
Carcinoid syndrome
Thyroid (>90%)
Medullary thyroid cancer (MTC)
Adrenal medulla (40-50%) Pheochromocytoma (40-50%)
Parathyroid (10-20%)
1o parathyroid hyperplasia
Skin
Cutaneous lichen amyloidosis
Thyroid
MTC (≥95%)
Thyroid MTC
Adrenal medulla Pheochromocytoma (≥50%)
Neurons
Mucosal neuroma, intestinal ganglioneuromas (100%)
MSK (100%)
Clinical Manifestations
Headache, visual field defects, often non- secreting but may secrete GH (acromegaly) and PRL (galactorrhea, erectile dysfunction, decreased libido, amenorrhea)
Nephrolithiasis, bone abnormalities, MSK complaints, symptoms of hypercalcemia
Epigastric pain (peptic ulcers and esophagitis) Hypoglycemia
Secretory diarrhea
Rash, anorexia, anemia, diarrhea, glossitis Flushing, diarrhea, bronchospasm
Physical signs are variable and often subtle
Neck mass or thyroid nodule; non-tender, anterior lymph nodes
HTN, palpitations, headache, sweating Symptoms of hypercalcemia
Scaly skin rash
MTC without other clinical manifestations of MEN IIa or IIb
MTC: most common component, more aggressive and earlier onset than MEN IIa HTN, palpitations, headache, sweating
Chronic constipation; megacolon Marfanoid habitus (no aortic abnormalities)
MEN II (chromosome 10) 1. IIa Sipple’s Syndrome
2. Familial Medullary Thyroid Ca (a variant of IIa)
3. IIb