Page 339 - TNFlipTest
P. 339
Toronto Notes 2019 Common Presenting Problems Osteoporosis
• seeEndocrinology,E41
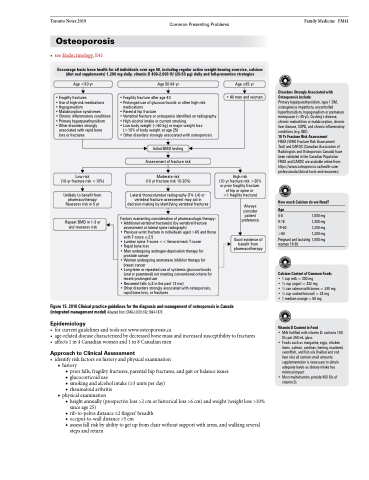
Encourage basic bone health for all individuals over age 50, including regular active weight-bearing exercise, calcium (diet and supplements) 1,200 mg daily, vitamin D 800-2,000 IU (20-50 μg) daily and fall-prevention strategies
Family Medicine FM41
Disorders Strongly Associated with Osteoporosis Include:
Primary hyperparathyroidism, type 1 DM, osteogenesis imperfecta, uncontrolled hyperthyroidism, hypogonadism or premature menopause (<45 yr), Cushing’s disease, chronic malnutrition or malabsorption, chronic liver disease, COPD, and chronic inflammatory conditions (e.g. IBD)
10 Yr Fracture Risk Assessment
FRAX (WHO Fracture Risk Assessment Tool) and CAROC (Canadian Association of Radiologists and Osteoporosis Canada) have been validated in the Canadian Population FRAX and CAROC are available online from: https://www.osteoporosis.ca/health-care- professionals/clinical-tools-and-resources/
How much Calcium do we Need?
Age
4-8 1,000 mg 9-18 1,300 mg 19-50 1,200 mg >50 1,200 mg Pregnant and lactating 1,000 mg women 19-50
Calcium Content of Common Foods
• 1cupmilk=300mg •3⁄4cupyogurt=332mg
• 1⁄2 can salmon with bones = 240 mg • 1⁄2 cup cooked broccoli = 33 mg
• 1 medium orange = 50 mg
Vitamin D Content in Food
• Milk fortified with vitamin D3 contains 100 IUs per 250 mL glass
• Foods such as margarine, eggs, chicken livers, salmon, sardines, herring, mackerel, swordfish, and fish oils (halibut and cod liver oils) all contain small amounts; supplementation is necessary to obtain adequate levels as dietary intake has minimal impact
• Most multivitamins provide 400 IUs of vitamin D3
Age <50 yr
• Fragility fractures
• Use of high-risk medications
• Hypogonadism
• Malabsorption syndromes
• Chronic inflammatory conditions
• Primary hyperparathyroidism
• Other disorders strongly
associated with rapid bone loss or fractures
Low risk
(10-yr fracture risk <10%)
Unlikely to benefit from pharmacotherapy Reassess risk in 5 yr
Repeat BMD in 1-3 yr and reassess risk
Age 50-64 yr
• Fragility fracture after age 40
• Prolonged use of glucocorticoids or other high-risk
medications
• Parental hip fracture
• Vertebral fracture or osteopenia identified on radiography • High alcohol intake or current smoking
• Low body weight (<60 kg) or major weight loss
(>10% of body weight at age 25)
• Other disorders strongly associated with osteoporosis
Initial BMD testing Assessment of fracture risk
Moderate risk
(10 yr fracture risk 10-20%)
Lateral thoracolumbar radiography (T4- L4) or vertebral fracture assessment may aid in decision-making by identifying vertebral fractures
Factors warranting consideration of pharmacologic therapy: • Additional vertebral fracture(s) (by vertebral fracture
assessment or lateral spine radiograph)
• Previous wrist fracture in individuals aged >65 and those
with T-score ≤-2.5
• Lumbar spine T-score << femoral neck T-score • Rapid bone loss
• Men undergoing androgen-deprivation therapy for
prostate cancer
• Women undergoing aromatase inhibitor therapy for
breast cancer
• Long-term or repeated use of systemic glucocorticoids
(oral or parenteral) not meeting conventional criteria for
recent prolonged use
• Recurrent falls (≤2 in the past 12 mo)
• Other disorders strongly associated with osteoporosis,
rapid bone loss, or fractures
Age ≥65 yr
• All men and women
High risk
(10 yr fracture risk >20% or prior fragility fracture of hip or spine or
>1 fragility fracture)
Always consider patient preference
Good evidence of benefit from pharmacotherapy
Figure 15. 2010 Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada (integrated management model) Adapted from: CMAJ 2010;182:1864-1873
Epidemiology
• forcurrentguidelinesandtoolsseewww.osteoporosis.ca
• age-relateddiseasecharacterizedbydecreasedbonemassandincreasedsusceptibilitytofractures • affects1in4Canadianwomenand1in8Canadianmen
Approach to Clinical Assessment
• identifyriskfactorsonhistoryandphysicalexamination ■ history
◆ prior falls, fragility fractures, parental hip fractures, and gait or balance issues ◆ glucocorticoid use
◆ smoking and alcohol intake (≥3 units per day)
◆ rheumatoid arthritis
■ physical examination
◆ height annually (prospective loss >2 cm or historical loss >6 cm) and weight (weight loss >10%
since age 25)
◆ rib-to-pelvis distance ≤2 fingers’ breadth
◆ occiput-to-wall distance >5 cm
◆ assess fall risk by ability to get up from chair without support with arms, and walking several
steps and return