Page 447 - TNFlipTest
P. 447
Toronto Notes 2019 Liver General Surgery and Thoracic Surgery GS45
■ non-surgical: radiofrequency ablation, percutaneous ethanol injection, transcatheter arterial chemoembolization (TACE), chemotherapy (consider sorafenib for HCC; pre-operative chemotherapy for hepatoblastoma is standard of care), and radiotherapy
• prognosis
■ median survival: 6-20 mo
■ 5 yr survival: 5% of all patients; 11-40% of patients undergoing complete resection
Secondary
• metastasestotheliverarethemostcommonmalignanttumoursfoundintheliver • etiology
■ GI (colorectal most common), lung, breast, pancreas, ovary, uterus, kidney, gallbladder, and prostate • treatment
■ depends on the primary cancer site and prognosis
◆ often liver metastases are a manifestation of Stage IV disease, and chemotherapy is indicated
■ metastasectomy may be appropriate for some cancers
◆ hepatic resection of metastatic colorectal liver metastases is standard of care as part of multi-
modality treatment that includes chemotherapy if complete resection of the primary cancer and
metastases is possible
◆ prognosis following liver resection for colorectal metastases is an overall survival of 30-60% at 5 yr
Secondary liver metastases are common in many cancers, with some studies showing a prevalence of 40-50% amongst patients with extrahepatic cancers. They commonly arise from breast, lung, and colorectal cancers. For metastases secondary to colorectal cancer, surgical resection offers the greatest likelihood of cure
Living Liver Donors vs. Deceased Liver Donors
The right lobe of a living donor liver is transplanted into the recipient, whereas whole livers from deceased donors are transplanted orthotopically into the recipient
Which Matters Most: Number of Tumours, Size of the Largest Tumour, or Total Tumour Volume? Liver Transplant 2011;17:S58-66
Purpose: To determine if the size and/or number of hepatocellular carcinoma (HCC) nodules
predict disease recurrence and survival after liver transplantation.
Methods: Systematic review and meta-analysis. Results: 74 studies were included for analysis. Patients beyond the Milan criteria had reduced overall and disease-free survivals and higher recurrence. Patients outside the UCSF criteria had reduced overall and disease-free survivals and higher recurrence. Patients outside the Milan criteria but within the UCSF criteria had reduced overall and disease-free survivals. Overall and disease-free survivals were reduced for patients with larger total tumour diameter, ≥10 cm vs. <10 cm and ≥9 cm vs. <9 cm, respectively. Similarly, patients with higher diameter of largest tumour nodule (≥3 cm vs. <3 cm) had reduced overall survival and higher recurrence. Overall and disease-free survivals were reduced and recurrence higher for patients with tumour size ≥5 cm vs. <5 cm. Mixed results were found regarding number of tumour nodules. Conclusion: Tumour size and volume are important factors in survival after liver transplantation.
Living Donor Liver Transplantation vs. Deceased Donor Liver Transplantation for Hepatocellular Carcinoma: Comparable Survival and Recurrence Liver Transplant 2012;18:315-322
Purpose: To compare the overall survival and hepatocellular carcinoma (HCC) recurrence rates after living donor liver transplantation (LDLT) versus deceased donor liver transplantation (DDLT) in a series of patients with HCC.
Methods: Study conducted between 1996 and 2009 at a single centre. 345 patients with HCC undergoing liver transplantation included.
Results: The overall survival rates at 1, 3, and 5
yr did not significantly differ between the LDLT
and DDLT groups (p=0.62). Disease free survival
at 1, 3, and 5 yr did not differ between the groups (p=0.82). The recurrence rates at 1, 3, and 5 yr also did not differ between the two group (p=0.54). Conclusion: LDLT and DDLT lead to similar survival and recurrence rates.
Liver Transplantation
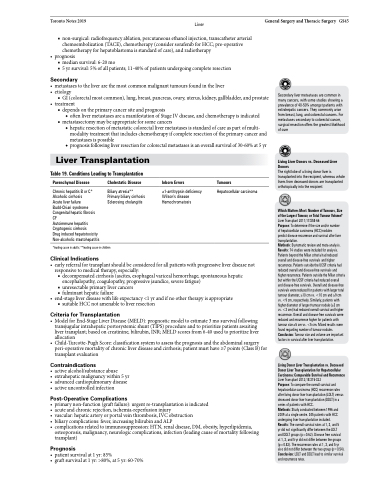
Table 19. Conditions Leading to Transplantation
Parenchymal Disease
Chronic hepatitis B or C* Alcoholic cirrhosis
Acute liver failure Budd-Chiari syndrome Congenital hepatic fibrosis CF
Autoimmune hepatitis Cryptogenic cirrhosis
Drug induced hepatotoxicity Non-alcoholic steatohepatitis
Cholestatic Disease
Biliary atresia** Primary biliary cirrhosis Sclerosing cholangitis
Inborn Errors
α1-antitrypsin deficiency Wilson’s disease Hemochromatosis
Tumours
Hepatocellular carcinoma
*leading cause in adults; **leading cause in children
Clinical Indications
• earlyreferralfortransplantshouldbeconsideredforallpatientswithprogressiveliverdiseasenot responsive to medical therapy, especially:
■ decompensated cirrhosis (ascites, esophageal variceal hemorrhage, spontaneous hepatic encephalopathy, coagulopathy, progressive jaundice, severe fatigue)
■ unresectable primary liver cancers
■ fulminant hepatic failure
• end-stageliverdiseasewithlifeexpectancy<1yrandifnoothertherapyisappropriate
■ suitable HCC not amenable to liver resection
Criteria for Transplantation
• ModelforEnd-StageLiverDisease(MELD):prognosticmodeltoestimate3mosurvivalfollowing transjugular intrahepatic portosystemic shunt (TIPS) procedure and to prioritize patients awaiting liver transplant; based on creatinine, bilirubin, INR; MELD scores from 6-40 used to prioritize liver allocation
• Child-Turcotte-PughScore:classificationsystemtoassesstheprognosisandtheabdominalsurgery peri-operative mortality of chronic liver disease and cirrhosis; patient must have ≥7 points (Class B) for transplant evaluation
Contraindications
• activealcohol/substanceabuse
• extrahepaticmalignancywithin5yr • advancedcardiopulmonarydisease • activeuncontrolledinfection
Post-Operative Complications
• primarynon-function(graftfailure):urgentre-transplantationisindicated • acute and chronic rejection, ischemia-reperfusion injury
• vascular:hepaticarteryorportalveinthrombosis,IVCobstruction
• biliarycomplications:fever,increasingbilirubinandALP
• complicationsrelatedtoimmunosuppression:HTN,renaldisease,DM,obesity,hyperlipidemia, osteoporosis, malignancy, neurologic complications, infection (leading cause of mortality following transplant)
Prognosis
• patientsurvivalat1yr:85%
• graftsurvivalat1yr:>80%,at5yr:60-70%