Page 464 - TNFlipTest
P. 464
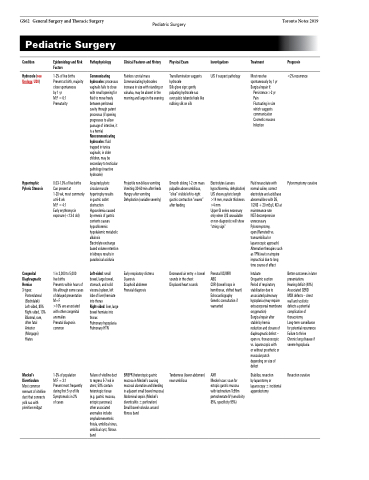
GS62 General Surgery and Thoracic Surgery Pediatric Surgery
Pediatric Surgery
Toronto Notes 2019
Condition
Hydrocele (see Urology, U30)
Epidemiology and Risk Factors
1-2% of live births Present at birth, majority close spontaneous by1yr
M:F = 6:1
Prematurity
Pathophysiology
Communicating hydroceles: processus vaginalis fails to close with small opening for fluid to move freely between peritoneal cavity through patent processus (if opening progresses to allow passage of intestine, it is a hernia) Noncommunicating hydroceles: fluid trapped in tunica vaginalis; in older children, may be secondary to testicular pathology (reactive hydrocele)
Acquired pyloric circular muscle hypertrophy results
in gastric outlet obstruction Hypovolemia caused by emesis of gastric contents causes hypochloremic hypokalemic metabolic alkalosis
Electrolyte exchange based volume retention in kidneys results in paradoxical aciduria
Left-sided: small bowel, large bowel, stomach, and solid viscera (spleen, left lobe of liver) herniate into thorax Right-sided: liver, large bowel herniate into thorax
Pulmonary hypoplasia Pulmonary HTN
Failure of vitelline duct to regress 5-7 wk in utero; 50% contain heterotopic tissue (e.g. gastric mucosa, ectopic pancreas); other associated anomalies include omphalomesenteric fistula, umbilical sinus, umbilical cyst, fibrous band
Clinical Features and History
Painless scrotal mass Communicating hydroceles increase in size with standing or valsalva, may be absent in the morning and large in the evening
Physical Exam
Transillumination suggests hydrocele
Silk glove sign: gently palpating hydrocele sac over pubic tubercle feels like rubbing silk on silk
Investigations
U/S if suspect pathology
Treatment
Most resolve spontaneously by 1 yr Surgical repair if:
Persistence >2 yr Pain
Fluctuating in size which suggests communication Cosmetic reasons Infection
Fluid resuscitate with normal saline, correct electrolyte and acid/base abnormalities with D5, 1/2NS + 20 mEq/L KCl at maintenance rate
NGT decompression unnecessary Pyloromyotomy,
open (Ramstedt vs. transumbilical or laparoscopic approach) Alternative therapies such as TPN/wait or atropine impractical due to long time course of effect
Intubate
Orogastric suction
Period of respiratory stabilization due to associated pulmonary hypoplasia (may require extracorporeal membrane oxygenation)
Surgical repair after stable by hernia reduction and closure of diaphragmatic defect – open vs. thoracoscopic vs. laparoscopic with
or without prosthetic or muscular patch depending on size of defect
Stabilize, resection
by laparotomy or laparoscopy ±incidental appendectomy
Prognosis
<2% recurrence
Hypertrophic Pyloric Stenosis
0.03-1.0% of live births Can present at
1-20 wk, most commonly at 6-8 wk
M:F = 4:1
Early erythromycin exposure (<13 d old)
1 in 2,000 to 5,000
live births
Presents within hours of life although some cases of delayed presentation M=F
>10% are associated with other congenital anomalies
Prenatal diagnosis common
1-3% of population
M:F = 3:1
Present most frequently during first 5 yr of life Symptomatic in 2%
of cases
Projectile non-bilious vomiting Vomiting 30-60 min after feeds Hungry after vomiting Dehydration (variable severity)
Early respiratory distress Cyanosis
Scaphoid abdomen Prenatal diagnosis
Smooth oblong 1-2 cm mass palpable above umbilicus, “olive” visible left-to-right gastric contraction “waves” after feeding
Decreased air entry ±bowel sounds in the chest Displaced heart sounds
Electrolytes (assess hypochloremia, dehydration) U/S shows pyloric length >14 mm, muscle thickness >4 mm
Upper GI series necessary only when U/S unavailable or non-diagnostic will show “string sign”
Prenatal US/MRI
ABG
CXR (bowel loops in hemithorax, shifted heart) Echocardiography Genetic consultation if warranted
AXR
Meckel scan: scan for ectopic gastric mucosa with technetium Tc99m pertechnetate IV (sensitivity 85%, specificity 95%)
Pyloromyotomy curative
Congenital Diaphragmatic Hernias
3 types:
Posterolateral (Bochdalek) Left-sided, 85% Right-sided, 13% Bilateral, rare, often fatal Anterior (Morgagni) Hiatus
Meckel’s Diverticulum Most common remnant of vitelline duct that connects yolk sac with primitive midgut
BRBPR (heterotopic gastric mucosa in Meckel’s causing mucosal ulceration and bleeding in adjacent small bowel mucosa) Abdominal sepsis (Meckel’s diverticulitis ±perforation) Small bowel volvulus around fibrous band
Tenderness (lower abdomen) near umbilicus
Better outcomes in later presentations
Hearing deficit (40%) Associated GERD
MSK defects – chest wall and scoliotic defects a potential complication of thoracotomy Long-term surveillance for potential recurrence Failure to thrive Chronic lung disease if severe hypoplasia
Resection curative