Page 465 - TNFlipTest
P. 465
Toronto Notes 2019
Pediatric Surgery
General Surgery and Thoracic Surgery GS63
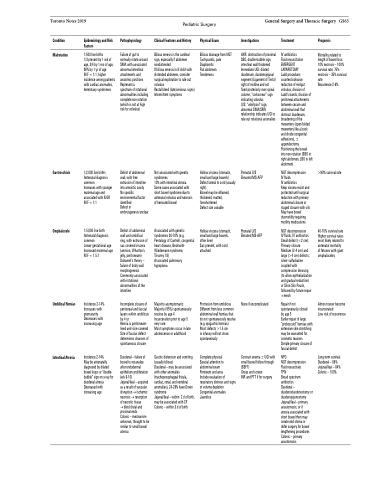
Condition
Malrotation
Epidemiology and Risk Factors
1:500 live births
1/3 present by 1 wk of age, 3/4 by 1 mo of age, 90% by 1 yr of age
M:F = 1:1; higher incidence among patients with cardiac anomalies, heterotaxy syndromes
Pathophysiology
Failure of gut to normally rotate around SMA with associated abnormal intestinal attachments and anatomic positions Represent a
spectrum of rotational abnormalities including complete non-rotation (which is not at high risk for volvulus)
Defect of abdominal wall, with free extrusion of intestine into amniotic cavity No specific environmental factor identified
Defect in embryogenesis unclear
Defect of abdominal wall and umbilical ring, with extrusion of sac covered viscera (amnion, Wharton’s jelly, peritoneum) Duhamel’s theory – failure of body wall morphogenesis Commonly associated with rotational abnormalities of the intestine
Incomplete closure of peritoneal and fascial layers within umbilicus by 4 yr
Hernia is peritoneum- lined and skin-covered Size of fascial defect determines chances of spontaneous closure
Duodenal – failure of bowel to recanalize after endodermal epithelium proliferation (wk 8-10)
Jejunal/ileal – acquired as a result of vascular disruption →ischemic necrosis →resorption of necrotic tissue
→ blind distal and proximal ends
Colonic – mechanism unknown, thought to be similar to small bowel atresia
Clinical Features and History
Bilious emesis is the cardinal sign, especially if abdomen nondistended
If bilious emesis in ill child with distended abdomen, consider surgical exploration to rule out volvulus
Rectal bleed (late/ominous signs) Intermittent symptoms
Physical Exam
Bilious drainage from NGT Tachycardic, pale Diaphoretic
Flat abdomen
Tenderness
Investigations
AXR: obstruction of proximal SBO, double-bubble sign, intestinal wall thickened Immediate UGI: dilated duodenum, duodenojejunal segment (Ligament of Treitz) right of midline and not fixed posteriorly over spinal column, “corkscrew” sign indicating volvulus
U/S: “whirlpool” sign, abnormal SMA/SMV relationship indicates UGI to rule out rotational anomalies
Prenatal U/S Elevated MS-AFP
Prenatal U/S Elevated MS-AFP
None if uncomplicated
Contrast enema ±UGI with small bowel follow through (SBFT)
Group and screen
INR and PTT if for surgery
Treatment
IV antibiotics
Fluid resuscitation EMERGENT LAPAROTOMY
Ladd procedure: counterclockwise reduction of midgut volvulus, division of Ladd’s bands, division of peritoneal attachments between cecum and abdominal wall that obstruct duodenum, broadening of the mesentery (open folded mesentery like a book and divide congenital adhesions), ± appendectomy Positioning the bowel into non-rotation (SBO in right abdomen, LBO in left abdomen)
NGT decompression
IV fluids
IV antibiotics
Keep viscera moist and protected until surgical reduction with primary abdominal closure or staged closure with silo May have bowel dysmotility requiring motility medications
NGT decompression
IV fluids, IV antibiotics Small defect (<2 cm): Primary closure Medium (2-4 cm) and large (>4 cm) defects: silver sulfadiazine coupled with compression dressing (to allow epithelialization and gradual reduction) or Silon Silo Pouch, followed by future repair ±mesh
Repair if not spontaneously closed
by age 5
Earlier repair of large “proboscoid” hernias with extensive skin stretching may be warranted for cosmetic reasons
Simple primary closure of fascial defect
NPO
NGT decompression Fluid resuscitate
TPN
Broad spectrum antibiotics
Duodenal – duodenoduodenostomy or duodenojejunostomy Jejunal/ileal – primary anastomosis; or if
atresia associated with short bowel then may create end stoma or defer surgery for bowel lengthening procedures Colonic – primary anastomosis
Prognosis
Mortality related to length of bowel loss: 10% necrosis – 100% survival rate, 75% necrosis – 35% survival rate
Recurrence 2-6%
Gastroschisis
Omphalocele
Umbilical Hernias
Intestinal Atresia
1:2,000 live births Antenatal diagnosis common
Increases with younger maternal age and associated with IUGR M:F = 1:1
1:5,000 live birth Antenatal diagnosis common
Lower gestational age Increased maternal age M:F = 1.5:1
Incidence 2-14% Increases with prematurity Decreases with increasing age
Incidence 2-14%
May be antenatally diagnosed by dilated bowel loops or “double- bubble” sign on x-ray for duodenal atresia Decreased with increasing age
Not associated with genetic syndromes
10% with intestinal atresia Some cases associated with short bowel syndrome due to antenatal volvulus and necrosis of herniated bowel
Associated with genetic syndromes 30-70% (e.g. Pentalogy of Cantrell, congenital heart disease, Beckwith- Wiedemann syndrome, Trisomy 18)
Associated pulmonary hypoplasia
Majority asymptomatic Majority (95%) spontaneously resolve by age 4 Incarceration prior to age 5 very rare
Most symptoms occur in late adolescence or adulthood
Gastric distension and vomiting (usually bilious)
Duodenal – may be associated with other anomalies (tracheoesophageal fistula, cardiac, renal, and vertebral anomalies), 24-28% have Down syndrome
Jejunal/ileal – within 2 d of birth, may be associated with CF Colonic – within 3 d of birth
Hollow viscera (stomach, small and large bowels) Defect lateral to cord (usually right)
Bowel may be inflamed, thickened, matted, foreshortened
Defect size variable
Hollow viscera (stomach, small and large bowels, often liver)
Sac present, with cord attached
Protrusion from umbilicus Different from less common abdominal wall hernias that do not spontaneously resolve (e.g. epigastric hernias) Most defects >1.5 cm
in infancy will not close spontaneously
Complete physical
Special attention to abdominal exam
Perineum and anus
Include evaluation of respiratory distress and signs of volume depletion Congenital anomalies Jaundice
>90% survival rate
40-70% survival rate Higher survival rates most likely related to antenatal mortality of fetuses with giant omphaloceles
Almost never become incarcerated
Low risk of recurrence
Long-term survival Duodenal – 86% Jejunal/ileal – 84% Colonic – 100%