Page 507 - TNFlipTest
P. 507
Toronto Notes 2019
Ectopic Pregnancy
Gynecology GY21
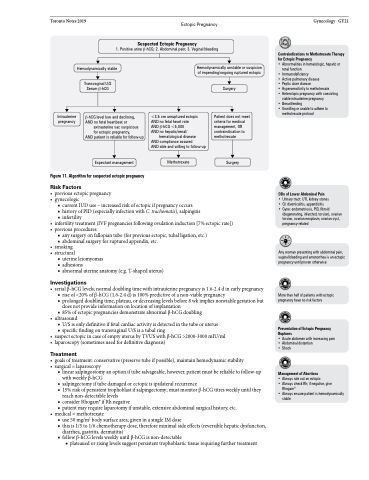
Suspected Ectopic Pregnancy
1. Positive urine β-hCG; 2. Abdominal pain; 3. Vaginal bleeding
Contraindications to Methotrexate Therapy for Ectopic Pregnancy
• Abnormalities in hematologic, hepatic or
renal function
• Immunodeficiency
• Active pulmonary disease
• Peptic ulcer disease
• Hypersensitivity to methotrexate
• Heterotopic pregnancy with coexisting
viable intrauterine pregnancy
• Breastfeeding
• Unwilling or unable to adhere to
methotrexate protocol
DDx of Lower Abdominal Pain
• Urinary tract: UTI, kidney stones
• GI: diverticulitis, appendicitis
• Gyne: endometriosis, PID, fibroid
(degenerating, infarcted, torsion), ovarian torsion, ovarian neoplasm, ovarian cyst, pregnancy-related
Any woman presenting with abdominal pain, vaginal bleeding and amenorrhea is an ectopic pregnancy until proven otherwise
More than half of patients with ectopic pregnancy have no risk factors
Presentation of Ectopic Pregnancy Ruptures
• Acute abdomen with increasing pain • Abdominal distention
• Shock
Management of Abortions
• Always rule out an ectopic
• Always check Rh; if negative, give
Rhogam®
• Always ensure patient is hemodynamically
stable
Hemodynamically stable
Transvaginal U/S Serum β-hCG
β-hCG level low and declining, AND no fetal heartbeat or
extrauterine sac suspicious
for ectopic pregnancy,
AND patient is reliable for follow-up
Expectant management
Hemodynamically unstable or suspicion of impending/ongoing ruptured ectopic
Intrauterine pregnancy
<3.5 cm unruptured ectopic AND no fetal heart rate
AND β-hCG <5,000
AND no hepatic/renal/
hematological disease
AND compliance assured
AND able and willing to follow-up
Methotrexate
Surgery
Patient does not meet criteria for medical management, OR contraindication to methotrexate
Surgery
Figure 11. Algorithm for suspected ectopic pregnancy
Risk Factors
• previousectopicpregnancy • gynecologic
■ current IUD use – increased risk of ectopic if pregnancy occurs
■ history of PID (especially infection with C. trachomatis), salpingitis ■ infertility
• infertilitytreatment(IVFpregnanciesfollowingovulationinduction[7%ectopicrate]) • previousprocedures
■ any surgery on fallopian tube (for previous ectopic, tubal ligation, etc.)
■ abdominal surgery for ruptured appendix, etc. • smoking
• structural
■ uterine leiomyomas
■ adhesions
■ abnormal uterine anatomy (e.g. T-shaped uterus)
Investigations
• serialβ-hCGlevels;normaldoublingtimewithintrauterinepregnancyis1.6-2.4dinearlypregnancy ■ rise of <20% of β-hCG (1.6-2.4 d) is 100% predictive of a non-viable pregnancy
■ prolonged doubling time, plateau, or decreasing levels before 8 wk implies nonviable gestation but
does not provide information on location of implantation
■ 85% of ectopic pregnancies demonstrate abnormal β-hCG doubling
• ultrasound
■ U/S is only definitive if fetal cardiac activity is detected in the tube or uterus ■ specific finding on transvaginal U/S is a tubal ring
• suspectectopicincaseofemptyuterusbyTVUSwithβ-hCG>2000-3000mIU/ml • laparoscopy(sometimesusedfordefinitivediagnosis)
Treatment
• goalsoftreatment:conservative(preservetubeifpossible),maintainhemodynamicstability • surgical=laparoscopy
■ linear salpingostomy an option if tube salvageable, however, patient must be reliable to follow-up with weekly β-hCG
■ salpingectomy if tube damaged or ectopic is ipsilateral recurrence
■ 15% risk of persistent trophoblast if salpingectomy; must monitor β-hCG titres weekly until they
reach non-detectable levels
■ consider Rhogam® if Rh negative
■ patient may require laparotomy if unstable, extensive abdominal surgical history, etc.
• medical=methotrexate
■ use 50 mg/m2 body surface area; given in a single IM dose
■ this is 1/5 to 1/6 chemotherapy dose, therefore minimal side effects (reversible hepatic dysfunction,
diarrhea, gastritis, dermatitis)
■ follow β-hCG levels weekly until β-hCG is non-detectable
◆ plateaued or rising levels suggest persistent trophoblastic tissue requiring further treatment