Page 524 - TNFlipTest
P. 524
GY38 Gynecology
Gynecological Oncology
Toronto Notes 2019
Gynecological Oncology
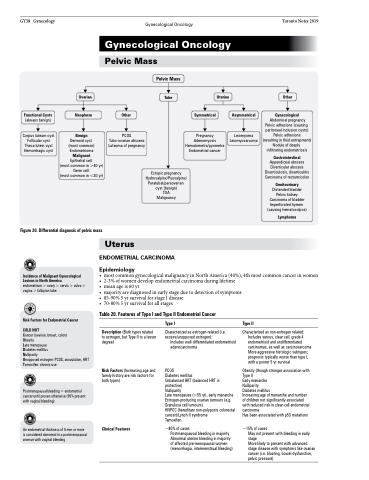
Pelvic Mass
Ovarian
Neoplasm Benign
Dermoid cyst
(most common) Endometrioma Malignant Epithelial cell
(most common in >40 yr) Germ cell
(most common in <20 yr)
Pelvic Mass
Tube
Uterine
Pregnancy Adenomyosis Hematometra/pyometra Endometrial cancer
Other
Gynecological
Abdominal pregnancy Pelvic adhesions (causing peritoneal inclusion cysts) Pelvic adhesions (resulting in fluid entrapment) Nodule of deeply infiltrating endometriosis
Gastrointestinal
Appendiceal abscess Diverticular abscess Diverticulosis, diverticulitis Carcinoma of rectum/colon
Genitourinary
Distended bladder Pelvic kidney Carcinoma of bladder Imperforated hymen (causing hematocolpos)
Lymphoma
Functional Cysts
(always benign)
Corpus luteum cyst Follicular cyst Theca lutein cyst Hemorrhagic cyst
Other
PCOS Tubo-ovarian abscess Luteoma of pregnancy
Symmetrical
Asymmetrical
Leiomyoma Leiomyosarcoma
Figure 20. Differential diagnosis of pelvic mass
Ectopic pregnancy Hydrosalpinx/Pyosalpinx/ Paratubal/paraovarian cyst (benign)
TOA Malignancy
Uterus
ENDOMETRIAL CARCINOMA
Epidemiology
Incidence of Malignant Gynecological Lesions in North America
endometrium > ovary > cervix > vulva > vagina > fallopian tube
Risk Factors for Endometrial Cancer COLD NUT
Cancer (ovarian, breast, colon) Obesity
Late menopause
Diabetes mellitus
• most common gynecological malignancy in North America (40%); 4th most common cancer in women • 2-3% of women develop endometrial carcinoma during lifetime
• meanageis60yr
• majorityarediagnosedinearlystageduetodetectionofsymptoms
• 85-90%5yrsurvivalforstageIdisease • 70-80%5yrsurvivalforallstages
Table 20. Features of Type I and Type II Endometrial Cancer
Nulliparity
Unopposed estrogen: PCOS, anovulation, HRT Tamoxifen: chronic use
Postmenopausal bleeding = endometrial cancer until proven otherwise (95% present with vaginal bleeding)
An endometrial thickness of 5 mm or more is considered abnormal in a postmenopausal woman with vaginal bleeding
Description (Both types related to estrogen, but Type II to a lesser degree)
Risk Factors (Increasing age and family history are risk factors for both types)
Clinical Features
Type I
Characterized as estrogen-related (i.e. excess/unopposed estrogen):
Includes well-differentiated endometrioid adenocarcinoma
PCOS
Diabetes mellitus
Unbalanced HRT (balanced HRT is protective)
Nulliparity
Late menopause (>55 yr), early menarche Estrogen-producing ovarian tumours (e.g. Granulosa cell tumours)
HNPCC (hereditary non-polyposis colorectal cancer)/Lynch II syndrome
Tamoxifen
~80% of cases
Postmenopausal bleeding in majority Abnormal uterine bleeding in majority of affected pre-menopausal women (menorrhagia, intermenstrual bleeding)
Type II
Characterized as non-estrogen related: Includes serous, clear cell, grade 4 endometrioid and undifferentiated carcinomas, as well as carcinosarcoma More aggressive histologic subtypes; prognosis typically worse than type I, with a poorer 5 yr survival
Obesity (though stronger association with Type I)
Early menarche
Nulliparity
Diabetes mellitus
Increasing age of menarche and number of children not significantly associated with reduced risk in clear-cell endometrial carcinoma
Has been associated with p53 mutations
~15% of cases
May not present with bleeding in early stage
More likely to present with advanced stage disease with symptoms like ovarian cancer (i.e. bloating, bowel dysfunction, pelvic pressure)