Page 555 - TNFlipTest
P. 555
Toronto Notes 2019
Microcytic Anemia
Hematology H15
Iron Deficiency Anemia
• seePediatrics,P42
• mostcommoncauseofanemiainNorthAmerica
Etiology
• increaseddemand
■ increased physiological need for iron in the body (e.g. pregnancy)
• decreasedsupply:dietarydeficiencies(rarelytheonlyetiologyinthedevelopedworld)
■ cow’smilk(infantdiet),“teaandtoast”diet(elderly),absorptionimbalances,post-gastrectomy,
malabsorption (IBD of duodenum, celiac disease, autoimmune atrophic gastritis, and H.pylori infection) • increasedlosses
■ hemorrhage
◆ obvious causes: menorrhagia, abnormal uterine bleeding, and frank GI bleed ◆ occult: peptic ulcer disease, GI cancer
■ hemolysis
◆ chronic intravascular hemolysis (e.g. PNH, cardiac valve RBC fragmentation)
Clinical Features
• irondeficiencymaycausefatiguebeforeclinicalanemiadevelops • signs/symptomsofanemia:seeAnemia,H6
• brittle hair, nail changes (brittle, koilonychia)
• pica(appetitefornon-foodsubstancese.g.ice,paint,anddirt)
• restlesslegsyndrome
Investigations
• ironindices,includingsolubletransferrinreceptor
■ low ferritin (<18 μg/L) is diagnostic of iron deficiency
■ ferritin is an acute phase reactant and is elevated in the setting of inflammatory conditions and
liver disease; serum ferritin <100 μg/L in these settings is suggestive of iron deficiency, necessitating
further workup
• peripheralbloodfilm
■ hypochromic microcytosis: RBCs have low Hb levels due to lack of iron ■ pencil forms, anisocytosis
■ target cells
• bonemarrow(goldstandardbutrarelydone)
■ iron stain (Prussian blue) shows decreased iron in macrophages and in erythroid precursors
Plummer-Vinson Syndrome
• Dysphagia (esophageal) • Glossitis
• Iron deficiency anemia • Stomatitis
Iron deficiency anemia is a common presentation of chronic lower GI bleeds (right- sided colorectal cancer, angiodysplasia, etc.)
In males and in post-menopausal women, a GI workup is always warranted (gastroscopy,
colonoscopy)
(sideroblasts)
■ intermediate and late erythroblasts show micronormoblastic maturation
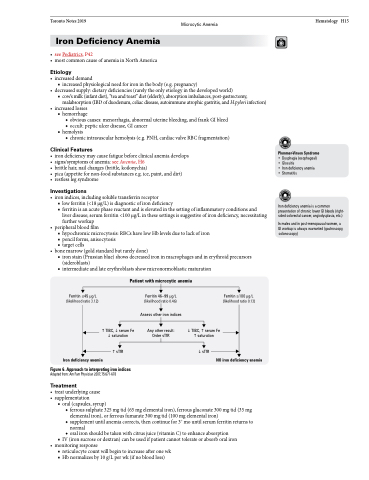
Patient with microcytic anemia
Ferritin ≤45 μg/L (likelihood ratio 3.12)
Ferritin 46–99 μg/L (likelihood ratio 0.46)
Assess other iron indices
Any other result: Order sTfR
Ferritin ≥100 μg/L (likelihood ratio 0.13)
sTfR Iron deficiency anemia
Figure 6. Approach to interpreting iron indices
Adapted from: Am Fam Physician 2007;75:671-678
Treatment
• treatunderlyingcause • supplementation
sTfR
NO iron deficiency anemia
TIBC,serum Fe saturation
TIBC,serum Fe saturation
■ oral (capsules, syrup)
◆ ferrous sulphate 325 mg tid (65 mg elemental iron), ferrous gluconate 300 mg tid (35 mg
elemental iron), or ferrous fumarate 300 mg tid (100 mg elemental iron)
◆ supplement until anemia corrects, then continue for 3+ mo until serum ferritin returns to
normal
◆ oral iron should be taken with citrus juice (vitamin C) to enhance absorption
■ IV (iron sucrose or dextran) can be used if patient cannot tolerate or absorb oral iron • monitoringresponse
■ reticulocyte count will begin to increase after one wk ■ Hb normalizes by 10 g/L per wk (if no blood loss)