Page 567 - TNFlipTest
P. 567
Toronto Notes 2019 Disorders of Primary Hemostasis
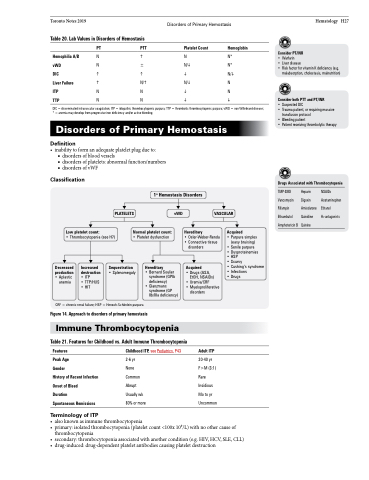
Table 20. Lab Values in Disorders of Hemostasis
Hematology H27
Hemophilia A/B vWD
DIC
Liver Failure ITP
TTP
PT PTT Platelet Count Hemoglobin
NhN N* N±N/i N* hhi N/i h N/h N/i N N NiN NNii
Consider PT/INR
• Warfarin
• Liver disease
• Risk factor for vitamin K deficiency (e.g.
malabsorption, cholestasis, malnutrition)
Consider both PTT and PT/INR
• Suspected DIC
• Trauma patient, or requiring massive
transfusion protocol
• Bleeding patient
• Patient receiving thrombolytic therapy
Drugs Associated with Thrombocytopenia
DIC = disseminated intravascular coagulation; ITP = idiopathic thrombocytopenic purpura; TTP = thrombotic thrombocytopenic purpura; vWD = von Willebrand disease; * = anemia may develop from progressive iron deficiency and/or active bleeding
Disorders of Primary Hemostasis
Definition
• inabilitytoformanadequateplateletplugdueto:
■ disorders of blood vessels
■ disorders of platelets: abnormal function/numbers ■ disorders of vWF
Classification
Low platelet count:
• Thrombocytopenia (see H7)
1o Hemostasis Disorders
TMP-SMX Vancomycin Rifampin Ethambutol Amphotericin B
Heparin NSAIDs Digoxin Acetaminophen Amiodarone Ethanol
PLATELETS
vWD VASCULAR
Quinidine Quinine
H2-antagonists
Normal platelet count:
• Platelet dysfunction
Hereditary
• Osler-Weber-Rendu • Connective tissue
disorders
Acquired
• Purpura simplex (easy bruising) • Senile purpura
• Dysproteinemias
• HSP
• Scurvy
• Cushing’s syndrome • Infections
• Drugs
Decreased production • Aplastic anemia
Increased Sequestration Hereditary Acquired
destruction
• ITP
• TTP/HUS • HIT
• Splenomegaly
• Bernard Soulier syndrome (GPIb deficiency)
• Glanzmans syndrome (GP IIb/IIIa deficiency)
• Drugs (ASA, EtOH, NSAIDs)
• Uremia/CRF
• Myeloproliferative
disorders
Adult ITP
20-40 yr F>M (3:1) Rare Insidious Mo to yr Uncommon
CRF = chronic renal failure; HSP = Henoch-Schönlein purpura
Figure 14. Approach to disorders of primary hemostasis
Immune Thrombocytopenia
Table 21. Features for Childhood vs. Adult Immune Thrombocytopenia
Features
Peak Age
Gender
History of Recent Infection Onset of Bleed
Duration
Spontaneous Remissions
Terminology of ITP
Childhood ITP, see Pediatrics, P43
2-6 yr
None Common Abrupt Usually wk 80% or more
• alsoknownasimmunethrombocytopenia
• primary:isolatedthrombocytopenia(plateletcount<100x109/L)withnoothercauseof
thrombocytopenia
• secondary:thrombocytopeniaassociatedwithanothercondition(e.g.HIV,HCV,SLE,CLL)
• drug-induced:drug-dependentplateletantibodiescausingplateletdestruction